Diagnosis and treatment of the portal vein complications for children undergoing spilt liver transplantation
-
摘要:
目的 探讨劈离式供肝儿童肝移植门静脉并发症的诊断及治疗策略。 方法 回顾性分析接受劈离式肝移植的88例儿童受者的临床资料。术中根据受者门静脉内径、发育情况,利用门静脉左右分支处进行吻合或间置供者髂静脉搭桥吻合,围手术期采用规范化的门静脉血流监测,术后按肝素钠桥接华法林的方案进行抗凝治疗。经增强CT或门静脉造影确诊门静脉狭窄或血栓形成后,予切开取栓、全身抗凝、介入下取栓、球囊扩张和(或)支架置入等处理。 结果 88例受者中共10例患儿确诊门静脉并发症,其中4例门静脉狭窄,确诊时间分别为术后1 d、2个月、8个月、11个月,6例门静脉血栓形成,确诊时间分别为术中、术后2 d、术后3 d(2例)、术后6 d、术后11个月。1例门静脉狭窄者和1例门静脉血栓形成者于围手术期死亡,门静脉并发症相关病死率为2%(2/88)。其余8例患者中,1例行全身抗凝治疗、2例行门静脉切开取栓术、1例行介入下球囊扩张、4例行介入下球囊扩张及支架置入,术后均长期随访,未再出现门静脉相关症状,复查门静脉血流参数正常。 结论 规范化的术中及术后门静脉血流监测有助于早期发现门静脉并发症,及时采取术中门静脉切开取栓,术后介入下球囊扩张、支架置入等手段可有效治疗门静脉并发症,减少门静脉并发症导致的移植物丢失和受者死亡。 Abstract:Objective To investigate the diagnosis and treatment strategy of the portal vein complications in children undergoing split liver transplantation. Methods The clinical data of 88 pediatric recipients who underwent split liver transplantation were retrospectively analyzed. Intraoperative anastomosis at the bifurcating site of the portal vein or donor iliac vein bypass anastomosis was performed depending on the internal diameter and development of the recipient's portal vein. A normalized portal venous blood stream monitoring was performed during the perioperative stage. After operation, heparin sodium was used to bridge warfarin for anticoagulation therapy. After portal vein stenosis or thrombosis was identified with enhanced CT or portography, managements including embolectomy, systemic anticoagulation, interventional thrombus removal, balloon dilatation and/or stenting were performed. Results Among the 88 recipients, a total of 10 children were diagnosed with portal vein complications, of which 4 cases were diagnosed with portal vein stenosis at 1 d, 2 months, 8 months, and 11 months after surgery, and 6 cases were diagnosed with portal vein thrombosis at intraoperative, 2 d, 3 d (n=2), 6 d, and 11 months after surgery, respectively. One patient with portal vein stenosis and one patient with portal vein thrombosis died perioperatively. The fatality related to portal vein complications was 2% (2/88). Of the remaining 8 patients, 1 underwent systemic anticoagulation, 2 underwent portal venous embolectomy, 1 underwent interventional balloon dilatation, and 4 underwent interventional balloon dilatation plus stenting. No portal venous related symptoms were detected during postoperative long term follow up, and the retested portal venous blood stream parameters were normal. Conclusions The normalized intra- and post-operative portal venous blood stream monitoring is a useful tool for the early detection of portal vein complications, the early utilization of useful managements such as intraoperative portal venous embolectomy, interventional balloon dilatation and stenting may effectively treat the portal vein complications, thus minimizing the portal vein complication related graft loss and recipient death. -
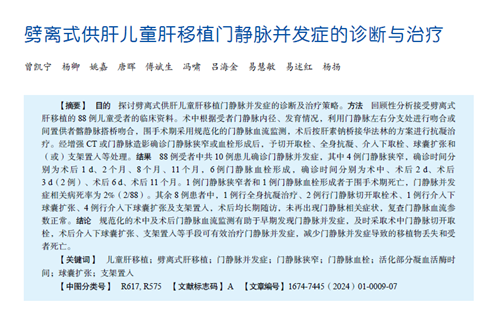
表 1 发生门静脉并发症的受者的临床资料
Table 1. Clinical data of recipients with portal venous complications
例序 性别 年龄 供者
血型受者
血型移植物类型 GRWR①
(%)并发症
类型诊断时间 处理方式 结局 随访时间 1 男 4岁2个月 A B 儿童右三叶 5.6 PVS 术后1 d 抗凝治疗 死亡 16 d 2 女 7个月 B AB 成人左半肝
(S2、S3减体积)3.8 PVS 术后2个月 抗凝治疗 无并发症生存 64个月 3 男 13岁5个月 O O 儿童右三叶 2.2 PVS 术后11个月 门静脉球囊扩张
(2次)+支架置入无并发症生存 61个月 4 男 6个月 B O 成人左外叶 3.2 PVS 术后8个月 门静脉球囊扩张
(2次)无并发症生存 57个月 5 男 9个月 O AB 成人左外叶 2.5 PVT 术后2 d 二次肝移植 死亡 8 d 6 男 4个月 A A 成人左外叶减体积 4.3 PVT 术中 门静脉切开取栓+
髂静脉间置搭桥无并发症生存 17个月 7 女 5个月 O A 成人左外叶 3.9 PVT 术后3 d 门静脉切开取栓 无并发症生存 64个月 8 女 1岁1个月 O O 成人左外叶减体积 3.3 PVT 术后3 d 门静脉球囊扩张+
支架置入无并发症生存 51个月 9 男 8个月 O B 儿童左外叶 2.6 PVT 术后6 d 门静脉球囊扩张+
支架置入无并发症生存 65个月 10 男 9个月 B O 儿童左外叶减体积 3.6 PVT 术后11个月 门静脉球囊扩张+
支架置入无并发症生存 14个月 注:①GRWR为移植物与受者质量比。 -
[1] BUELL JF, FUNAKI B, CRONIN DC, et al. Long-term venous complications after full-size and segmental pediatric liver transplantation[J]. Ann Surg, 2002, 236(5): 658-666. DOI: 10.1097/00000658-200211000-00017. [2] UEDA M, OIKE F, KASAHARA M, et al. Portal vein complications in pediatric living donor liver transplantation using left-side grafts[J]. Am J Transplant, 2008, 8(10): 2097-2105. DOI: 10.1111/j.1600-6143.2008.02360.x. [3] STEVENS JP, XIANG Y, LEONG T, et al. Portal vein complications and outcomes following pediatric liver transplantation: data from the Society of Pediatric Liver Transplantation[J]. Liver Transpl, 2022, 28(7): 1196-1206. DOI: 10.1002/lt.26412. [4] REN J, DONG C, SUN C, et al. The impact of portal vein reconstruction on portal vein complications after pediatric living-donor liver transplantation with left lobe graft[J]. Surgery, 2023, 173(2): 537-543. DOI: 10.1016/j.surg.2022.10.020. [5] ANOUTI A, PATEL MS, VANWAGNER LB, et al. Biliary atresia and liver transplantation in the United States: a contemporary analysis[J]. Liver Int, 2023, 43(10): 2198-2209. DOI: 10.1111/liv.15689. [6] LAUTERIO A, CILLO U, SPADA M, et al. Improving outcomes of in situ split liver transplantation in Italy over the last 25 years[J]. J Hepatol, 2023, 79(6): 1459-1468. DOI: 10.1016/j.jhep.2023.07.009. [7] ROKOP ZP, MANGUS RS, TOLLIVER K, et al. Comparative analysis of whole vs. split liver transplantation in infants[J]. Pediatr Transplant, 2023, 27(6): e14564. DOI: 10.1111/petr.14564. [8] XU M, DONG C, SUN C, et al. Impact of donor age on short-term outcomes after pediatric split liver transplantation[J]. Front Pediatr, 2023, 11: 1131629. DOI: 10.3389/fped.2023.1131629. [9] SMITH SK, MILOH T. Pediatric liver transplantation[J]. Clin Liver Dis, 2022, 26(3): 521-535. DOI: 10.1016/j.cld.2022.03.010. [10] 李姗霓, 孙超, 马楠, 等. 175例小儿肝移植门静脉重建技术的单中心经验总结[J/CD]. 实用器官移植电子杂志, 2014, 2(5): 279-282. DOI: 10.3969/j.issn.2095-5332.2014.05.004.LI SN, SUN C, MA N, et al. Portal vein reconstruction in 175 cases of pediatric liver transplantation: a single center experience[J/CD]. Pract J Organ Transplant(Electr Vers), 2014, 2(5): 279-282. DOI: 10.3969/j.issn.2095-5332.2014.05.004. [11] LEE J, YI NJ, KIM JY, et al. Portal vein reconstruction in pediatric liver transplantation using end-to-side jump graft: a case report[J]. Ann Hepatobiliary Pancreat Surg, 2023, 27(3): 313-316. DOI: 10.14701/ahbps.22-125. [12] 徐瑞芳, 何恩辉, 易展雄, 等. 儿童肝移植术后门静脉狭窄危险因素分析[J]. 中国医学装备, 2021, 18(7): 122-125. DOI: 10.3969/J.ISSN.1672-8270.2021.07.027.XU RF, HE EH, YI ZX, et al. Analysis on the risk factors of PVS after pediatric liver transplantation[J]. China Med Equip, 2021, 18(7): 122-125. DOI: 10.3969/J.ISSN.1672-8270.2021.07.027. [13] SAKAMOTO S, UCHIDA H, KITAJIMA T, et al. The outcomes of portal vein reconstruction with vein graft interposition in pediatric liver transplantation for small children with biliary atresia[J]. Transplantation, 2020, 104(1): 90-96. DOI: 10.1097/TP.0000000000002793. [14] NAMGOONG JM, HWANG S, PARK GC, et al. Modified patch-conduit venoplasty for portal vein hypoplasia in pediatric liver transplantation[J]. Korean J Transplant, 2023,DOI: 10.4285/kjt.23.0037[Epub ahead of print [15] BOILLOT O, GUILLAUD O, WISCHLEN E, et al. Determinants of early surgical complications after pediatric liver transplantation: a single center/single surgeon experience over 20 years[J]. Clin Res Hepatol Gastroenterol, 2023, 47(9): 102222. DOI: 10.1016/j.clinre.2023.102222. [16] RODRIGUEZ-DAVALOS MI, LOPEZ-VERDUGO F, KASAHARA M, et al. International liver transplantation society global census: first look at pediatric liver transplantation activity around the world[J]. Transplantation, 2023, 107(10): 2087-2097. DOI: 10.1097/TP.0000000000004644. [17] YU Z, KESKINOCAK P, MAGLIOCCA JF, et al. Split or whole liver transplantation? utilization and posttransplant survival[J]. Hepatol Commun, 2023, 7(9): e0225. DOI: 10.1097/HC9.0000000000000225. [18] DALZELL C, VARGAS PA, SOLTYS K, et al. Living donor liver transplantation vs. split liver transplantation using left lateral segment grafts in pediatric recipients: an analysis of the UNOS database[J]. Transpl Int, 2022, 36: 10437. DOI: 10.3389/ti.2022.10437. [19] BOWRING MG, MASSIE AB, SCHWARZ KB, et al. Survival benefit of split-liver transplantation for pediatric and adult candidates[J]. Liver Transpl, 2022, 28(6): 969-982. DOI: 10.1002/lt.26393. [20] SOLTYS K, LEMOINE C, ZHANG X, et al. Factors associated with thrombotic and hemorrhagic complications in pediatric liver transplant: a multi-center analysis from the Starzl Network for Excellence in Pediatric Transplantation[J]. Pediatr Transplant, 2023, 27(4): e14521. DOI: 10.1111/petr.14521. [21] SOLTYS KA, MAZARIEGOS GV, SQUIRES RH, et al. Late graft loss or death in pediatric liver transplantation: an analysis of the SPLIT database[J]. Am J Transplant, 2007, 7(9): 2165-2171. DOI: 10.1111/j.1600-6143.2007.01893.x. [22] XIE E, SUN C, DONG C, et al. Impact of allograft types on outcomes after pediatric liver transplantation due to biliary atresia[J]. Pediatr Transplant, 2022, 26(7): e14342. DOI: 10.1111/petr.14342. [23] WANG Z, GAO W, DONG C, et al. Outcome of split-liver transplantation from pediatric donors weighing 25 kg or less[J]. Liver Transpl, 2023, 29(1): 58-66. DOI: 10.1002/lt.26530. [24] YOON KC, SONG S, LEE S, et al. Outcomes of split liver transplantation vs living donor liver transplantation in pediatric patients: a 5-year follow-up study in Korea[J]. Ann Transplant, 2022, 27: e935682. DOI: 10.12659/AOT.935682. [25] 何志忠, 周路遥. 儿童肝移植术后门静脉狭窄的超声评估价值[J]. 器官移植, 2020, 11(6): 704-710. DOI: 10.3969/j.issn.1674-7445.2020.06.009.HE ZZ, ZHOU LY. Ultrasound evaluation value of portal vein stenosis after pediatric liver transplantation[J]. Organ Transplant, 2020, 11(6): 704-710. DOI: 10.3969/j.issn.1674-7445.2020.06.009. [26] CHANG NW, WANG HK, LIU CS, et al. First-pass arrival interval of ultrasound contrast medium in the hepatic artery and portal vein as a marker for assessment of liver transplant recipients[J]. Transplant Proc, 2021, 53(7): 2329-2334. DOI: 10.1016/j.transproceed.2021.07.050. [27] 尹超, 朱志军, 魏林, 等. 儿童肝移植术后门静脉狭窄的诊断与治疗[J/CD]. 中华移植杂志(电子版), 2019, 13(3): 219-223. DOI: 10.3877/cma.j.issn.1674-3903.2019.03.012.YIN C, ZHU ZJ, WEI L, et al. Diagnosis and treatment of portal vein stenosis after pediatric liver transplantation[J/CD]. Chin J Transplant (Electr Edit), 2019, 13(3): 219-223. DOI: 10.3877/cma.j.issn.1674-3903.2019.03.012. [28] 江波, 何恩辉, 钱林学, 等. 超声评估儿童肝移植后门静脉狭窄的诊断价值[J]. 临床和实验医学杂志, 2016, 15(24): 2429-2432. DOI: 10.3969/j.issn.1671-4695.2016.24.015.JIANG B, HE EH, QIAN LX, et al. Doppler sonography evaluation of postoperative portal vein stenosis in pediatric living donor liver transplantation[J]. J Clin Exp Med, 2016, 15(24): 2429-2432. DOI: 10.3969/j.issn.1671-4695.2016.24.015. [29] SLOWIK V, RYAN JL, SHAH AA, et al. Monitoring practices after pediatric liver transplantation[J]. J Pediatr Gastroenterol Nutr, 2023, 77(4): 448-454. DOI: 10.1097/MPG.0000000000003909. [30] 王晓静, 王岩青, 郭朝锋, 等. 肝移植术后门静脉并发症的超声检测价值[J]. 临床超声医学杂志, 2017, 19(5): 341-343. DOI: 10.3969/j.issn.1008-6978.2017.05.022.WANG XJ, WANG YQ, GUO CF, et al. Clinical value of color Doppler ultrasound in detection of portal vein complications after liver transplantation[J]. J Clin Ultrasound Med, 2017, 19(5): 341-343. DOI: 10.3969/j.issn.1008-6978.2017.05.022. [31] TAMSEL S, DEMIRPOLAT G, KILLI R, et al. Vascular complications after liver transplantation: evaluation with Doppler US[J]. Abdom Imaging, 2007, 32(3): 339-347. DOI: 10.1007/s00261-006-9041-z. [32] CHONG WK, BELAND JC, WEEKS SM. Sonographic evaluation of venous obstruction in liver transplants[J]. AJR Am J Roentgenol, 2007, 188(6): W515-W521. DOI: 10.2214/AJR.06.1262. [33] SAINZ-BARRIGA M, REYNTJENS K, COSTA MG, et al. Prospective evaluation of intraoperative hemodynamics in liver transplantation with whole, partial and DCD grafts[J]. Am J Transplant, 2010, 10(8): 1850-1860. DOI: 10.1111/j.1600-6143.2010.03207.x. [34] 武红涛, 唐缨, 胡翔宇. 活体肝移植术中门静脉血流量与术后肝功能恢复的相关性研究[J]. 中华超声影像学杂志, 2011, 20(1): 26-29. DOI: 10.3760/cma.j.issn.1004-4477.2011.01.008.WU HT, TANG Y, HU XY, et al. Correlation of portal vein flow in living donor right lobe liver transplantation and graft function post-operation studies by intraoperative Doppler ultrasonography[J]. Chin J Ultrason, 2011, 20(1): 26-29. DOI: 10.3760/cma.j.issn.1004-4477.2011.01.008. [35] 陈文忠, 张升宁, 钟粤明, 等. 肝移植术后门静脉系统并发症的血管内介入治疗[J]. 影像研究与医学应用, 2020, 4(13): 34-37. DOI: 10.3969/j.issn.2096-3807.2020.13.017.CHEN WZ, ZHANG SN, ZHONG YM, et al. Percutaneous intravascular interventional treatment of portal venous complications after liver transplantation[J]. J Imag Res Med Appl, 2020, 4(13): 34-37. DOI: 10.3969/j.issn.2096-3807.2020.13.017. [36] 陈光, 高海军. 儿童肝移植术后血管并发症的介入治疗[J/CD]. 实用器官移植电子杂志, 2016, 4(4): 246-247. DOI: 10.3969/j.issn.2095-5332.2016.04.012.CHEN G, GAO HJ. Interventional treatment of vascular complications after liver transplantation in children [J/CD]. Pract J Organ Transplant(Electr Vers) , 2016, 4(4): 246-247. DOI: 10.3969/j.issn.2095-5332.2016.04.012. [37] BUKOVA M, FUNKEN D, PFISTER ED, et al. Long-term outcome of primary percutaneous stent angioplasty for pediatric posttransplantation portal vein stenosis[J]. Liver Transpl, 2022, 28(9): 1463-1474. DOI: 10.1002/lt.26488. [38] VOULGARELIS S, VITOLA B, LERRET SM, et al. Perioperative anticoagulation practices for pediatric liver transplantation[J]. Pediatr Transplant, 2018, 22(4): e13193. DOI: 10.1111/petr.13193. [39] LEE S, YI NJ, HAN ES, et al. Long-term survival outcomes beyond the first year after liver transplantation in pediatric acute liver failure compared with biliary atresia: a large-volume living donor liver transplantation single-center study[J]. J Clin Med, 2022, 11(24): 7480. DOI: 10.3390/jcm11247480. [40] VERHAGEN MV, DE KLEINE RHJ, VAN DER DOEF HPJ, et al. Doppler ultrasound of vascular complications after pediatric liver transplantation: incidence, time of detection, and positive predictive value[J]. Ultrasound Int Open, 2022, 8(2): E36-E42. DOI: 10.1055/a-1961-9100. [41] SANADA Y, SAKUMA Y, ONISHI Y, et al. Long-term outcomes in pediatric patients who underwent living donor liver transplantation for biliary atresia[J]. Surgery, 2022, 171(6): 1671-1676. DOI: 10.1016/j.surg.2021.11.027. -





 下载:
下载: