-
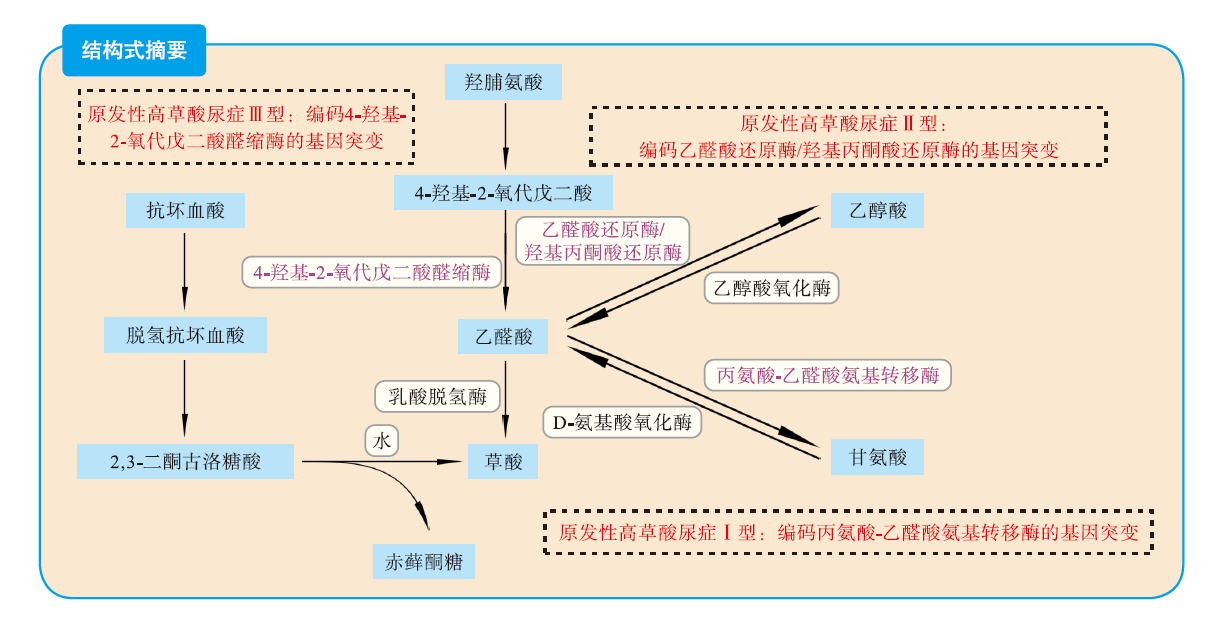
摘要: 原发性高草酸尿症Ⅱ型(PH2)是由乙醛酸还原酶/羟基丙酮酸还原酶(GRHPR)基因突变引起的乙醛酸代谢障碍性遗传病。其特征是复发性肾草酸钙结石和肾钙盐沉着症,严重者可进展至终末期肾病。器官移植是目前治愈PH2的唯一方法,主要包括肾移植和肝肾联合移植两种策略。前者有较高的草酸盐肾病复发风险,可能造成移植肾早期失功。后者能纠正草酸代谢缺陷,但具有较高的移植物并发症发生风险。由于PH2的罕见性,目前尚未就该疾病器官移植的指征、术式选择、围手术期管理等达成共识。本文就PH2的发病机制、诊断与监测以及器官移植经验做一综述,旨在引起临床医师对PH2的重视,并为PH2诊治方案尤其是移植策略的制定提供参考。
-
关键词:
- 原发性高草酸尿症Ⅱ型 /
- 肾结石 /
- 终末期肾病(ESRD) /
- 肾移植 /
- 肝肾联合移植 /
- 草酸钙结石
Abstract: Primary hyperoxaluria type Ⅱ (PH2) is an inherited disorder of the glyoxylate metabolism caused by the gene mutation of glyoxylate reductase/hydroxypyruvate reductase (GRHPR). PH2 is characterized by recurrent nephrolithiasis and nephrocalcinosis, which may even progress into end-stage renal disease. Currently, organ transplantation is the only treatment option for PH2, which mainly includes two strategies: kidney transplantation and combined liver and kidney transplantation. Kidney transplantation yields a high risk of recurrence of oxalate nephropathy, which may cause early graft dysfunction. Combined liver and kidney transplantation could mitigate the deficiency of oxalate metabolism, whereas it yields a high risk of graft complications. PH2 is an extremely rare disorder. No consensus has been reached on the indications, surgical selection and perioperative management of organ transplantation for PH2 patients. In this article, the pathogenesis, diagnosis, monitoring and organ transplantation experience of PH2 were reviewed, aiming to divert clinicians' attention to PH2 and provide reference for determining diagnosis and treatment regimens, especially transplantation strategy for PH2 patients. -
表 1 PH2患者器官移植策略及预后报道
Table 1. Organ transplantation strategies and prognosis of PH2 patients reported in literature
研究者 n 发病年龄(岁) 基因突变 移植年龄(岁) 手术指征 移植策略 术后随访时间(月) 结局 Garrelfs SF,
et al [14]6 -① - - - 肾移植5例
肝肾联合
移植1例12.0~264.0 1例肝肾联合移植受者死亡,其余5例移植肾均失功 Hosaagrahara Ramakrishna S, et al [15] 1 9 c.735-1G>A 12 CKD 5期,系统性草酸沉着症 肝肾联合
移植18.0 移植肾存活 Lam CW,
et al [28]1 4 c.862_863delTG - 双肾结石,CKD 5期 肾移植+双侧肾切除 - 移植肾存活 Naderi G,
et al [29]1 <5 - 9 CKD 5期 肾移植 11.0 移植肾失功、切除 Liu S, et al [30] 1 23 c.864_865delTG 33 CKD 5期 肾移植 1.6 移植肾失功、切除 Dhondup T,
et al [31]2 6 c.139C>T 37、44 急性肾衰竭、肾移植后移植肾衰竭 肾移植、肝肾联合移植 12.8、60.0 单独肾移植后移植肾失功,肝肾联合移植后移植肾存活 Del Bello A,
et al [32]1 22 c.103delG 41 CKD 5期 肾移植 6.0 移植肾失功 Del Bello A,
et al [33]1 22 c.103delG 43 肾移植后
移植肾衰竭肝肾联合
移植15.0 移植肾存活 Jia Z, et al [34] 1 - c.532_533delCA 26 CKD 5期,肾移植后草酸盐肾病复发 肾移植后
追加肝移植2.0 移植肾失功 Genena KM,
et al [35]1 18 c.103delG; c.781_782delinsTAC 30 CKD 5期 肝肾联合
移植12.0 移植肾存活 Yau AA,
et al [36]1 - c.494G>A 56 - 肾移植 >3.0 移植肾存活 Monico CG,
et al [37]1 - - 22 - 肾移植 242.4 移植肾存活 注:①-指文献未报道。
-
[1] 王心悦, 詹浩苏, 孙丽莹. 中国大陆原发性高草酸尿症1型临床特点及诊治情况总结[J]. 器官移植, 2022, 13(2): 232-239. DOI: 10.3969/j.issn.1674-7445.2022.02.012.WANG XY, ZHAN HS, SUN LY. Summary of clinical characteristics, diagnosis and treatment of primary hyperoxaluria type 1 in mainland China[J]. Organ Transplant, 2022, 13(2): 232-239. DOI: 10.3969/j.issn.1674-7445.2022.02.012. [2] SINGH P, VIEHMAN JK, MEHTA RA, et al. Clinical characterization of primary hyperoxaluria type 3 in comparison with types 1 and 2[J]. Nephrol Dial Transplant, 2022, 37(5): 869-875. DOI: 10.1093/ndt/gfab027. [3] SHEE K, STOLLER ML. Perspectives in primary hyperoxaluria - historical, current and future clinical interventions[J]. Nat Rev Urol, 2022, 19(3): 137-146. DOI: 10.1038/s41585-021-00543-4. [4] MANDRILE G, PELLE A, SCIANNAMEO V, et al. Primary hyperoxaluria in Italy: the past 30 years and the near future of a (not so) rare disease[J]. J Nephrol, 2022, 35(3): 841-850. DOI: 10.1007/s40620-022-01258-4. [5] SIKORA P, ZANIEW M, GRENDA R, et al. Still diagnosed too late and under-recognized? the first comprehensive report on primary hyperoxaluria in Poland[J]. Pol Arch Intern Med, 2020, 130(12): 1053-1063. DOI: 10.20452/pamw.15698. [6] CRIVELLI JJ, MITCHELL T, KNIGHT J, et al. Contribution of dietary oxalate and oxalate precursors to urinary oxalate excretion[J]. Nutrients, 2020, 13(1): 62. DOI: 10.3390/nu13010062. [7] CAPOLONGO G, FERRARO PM, UNWIN R. Inflammation and kidney stones: cause and effect?[J]. Curr Opin Urol, 2023, 33(2): 129-135. DOI: 10.1097/MOU.0000000000001066. [8] DEMOULIN N, AYDIN S, GILLION V, et al. Pathophysiology and management of hyperoxaluria and oxalate nephropathy: a review[J]. Am J Kidney Dis, 2022, 79(5): 717-727. DOI: 10.1053/j.ajkd.2021.07.018. [9] PIJNENBURG L, CAILLARD S, BOIVIN G, et al. Type 1 primary hyperoxaluria: a case report and focus on bone impairment of systemic oxalosis[J]. Morphologie, 2018, 102(336): 48-53. DOI: 10.1016/j.morpho.2017.09.004. [10] BIRTEL J, DIEDEREN RM, HERRMANN P, et al. The retinal phenotype in primary hyperoxaluria type 2 and 3[J]. Pediatr Nephrol, 2023, 38(5): 1485-1490. DOI: 10.1007/s00467-022-05765-1. [11] LEE DH, KASPROWICZ T, MORALES A, et al. A case of infiltrative cardiomyopathy secondary to primary hyperoxaluria type 2 - utilization of multimodality imaging[J]. Cureus, 2021, 13(9): e17914. DOI: 10.7759/cureus.17914. [12] DEVRESSE A, COCHAT P, GODEFROID N, et al. Transplantation for primary hyperoxaluria type 1: designing new strategies in the era of promising therapeutic perspectives[J]. Kidney Int Rep, 2020, 5(12): 2136-2145. DOI: 10.1016/j.ekir.2020.09.022. [13] COCHAT P, RUMSBY G. Primary hyperoxaluria[J]. N Engl J Med, 2013, 369(7): 649-658. DOI: 10.1056/NEJMra1301564. [14] GARRELFS SF, RUMSBY G, PETERS-SENGERS H, et al. Patients with primary hyperoxaluria type 2 have significant morbidity and require careful follow-up[J]. Kidney Int, 2019, 96(6): 1389-1399. DOI: 10.1016/j.kint.2019.08.018. [15] HOSAAGRAHARA RAMAKRISHNA S, HASSAN A, KASALA MB, et al. Pediatric combined living donor liver and kidney transplantation for primary hyperoxaluria type 2[J]. Am J Transplant, 2023, 23(10): 1622-1625. DOI: 10.1016/j.ajt.2023.05.006. [16] MANDRILE G, BECK B, ACQUAVIVA C, et al. Genetic assessment in primary hyperoxaluria: why it matters[J]. Pediatr Nephrol, 2023, 38(3): 625-634. DOI: 10.1007/s00467-022-05613-2. [17] 詹睿超, 葛玉成, 张道新, 等. 原发性高草酸尿症基因型与表型的研究进展[J]. 国际外科学杂志, 2021, 48(3): 203-207. DOI: 10.3760/cma.j.cn115396-20200319-00072.ZHAN RC, GE YC, ZHANG DX, et al. Research progress on genotype and phenotype of primary hyperoxaluria[J]. Int J Surg, 2021, 48(3): 203-207. DOI: 10.3760/cma.j.cn115396-20200319-00072. [18] GROOTHOFF JW, METRY E, DEESKER L, et al. Clinical practice recommendations for primary hyperoxaluria: an expert consensus statement from ERKNet and OxalEurope[J]. Nat Rev Nephrol, 2023, 19(3): 194-211. DOI: 10.1038/s41581-022-00661-1. [19] ZHAO F, BERGSTRALH EJ, MEHTA RA, et al. Predictors of incident ESRD among patients with primary hyperoxaluria presenting prior to kidney failure[J]. Clin J Am Soc Nephrol, 2016, 11(1): 119-126. DOI: 10.2215/CJN.02810315. [20] INJEYAN M, BIDAULT V, BACCHETTA J, et al. Hydration and nephrolithiasis in pediatric populations: specificities and current recommendations[J]. Nutrients, 2023, 15(3): 728. DOI: 10.3390/nu15030728. [21] 冯潇雨, 程娜, 张荣军, 等. 儿童原发性高草酸尿症1型1例并文献复习[J]. 中国临床研究, 2021, 34(9): 1245-1249. DOI: 10.13429/j.cnki.cjcr.2021.09.021.FENG XY, CHENG N, ZHANG RJ, et al. A case of primary hyperoxaluria type 1 in children and literature review[J]. Chin J Clin Res, 2021, 34(9): 1245-1249. DOI: 10.13429/j.cnki.cjcr.2021.09.021. [22] BHASIN B, ÜREKLI HM, ATTA MG. Primary and secondary hyperoxaluria: understanding the enigma[J]. World J Nephrol, 2015, 4(2): 235-244. DOI: 10.5527/wjn.v4.i2.235. [23] BOSE KS, SARMA RH. Delineation of the intimate details of the backbone conformation of pyridine nucleotide coenzymes in aqueous solution[J]. Biochem Biophys Res Commun, 1975, 66(4): 1173-1179. DOI: 10.1016/0006-291x(75)90482-9. [24] MASSY ZA, DRUEKE TB. Running interference: lumasiran and other RNA interference therapeutics for kidney diseases[J]. Kidney Int, 2022, 101(2): 208-211. DOI: 10.1016/j.kint.2021.05.027. [25] METRY EL, VAN DIJK LMM, PETERS-SENGERS H, et al. Transplantation outcomes in patients with primary hyperoxaluria: a systematic review[J]. Pediatr Nephrol, 2021, 36(8): 2217-2226. DOI: 10.1007/s00467-021-05043-6. [26] CORNELL LD, AMER H, VIEHMAN JK, et al. Posttransplant recurrence of calcium oxalate crystals in patients with primary hyperoxaluria: incidence, risk factors, and effect on renal allograft function[J]. Am J Transplant, 2022, 22(1): 85-95. DOI: 10.1111/ajt.16732. [27] GUPTA A, SOMERS MJG, BAUM MA. Treatment of primary hyperoxaluria type 1[J]. Clin Kidney J, 2022, 15(Suppl 1): i9-i13. DOI: 10.1093/ckj/sfab232. [28] LAM CW, YUEN YP, LAI CK, et al. Novel mutation in the GRHPR gene in a Chinese patient with primary hyperoxaluria type 2 requiring renal transplantation from a living related donor[J]. Am J Kidney Dis, 2001, 38(6): 1307-1310. DOI: 10.1053/ajkd.2001.29229. [29] NADERI G, LATIF A, TABASSOMI F, et al. Failure of isolated kidney transplantation in a pediatric patient with primary hyperoxaluria type 2[J]. Pediatr Transplant, 2014, 18(3): E69-E73. DOI: 10.1111/petr.12240. [30] LIU S, GAO B, WANG G, et al. Recurrent primary hyperoxaluria type 2 leads to early post-transplant renal function loss: a case report[J]. Exp Ther Med, 2018, 15(4): 3169-3172. DOI: 10.3892/etm.2018.5841. [31] DHONDUP T, LORENZ EC, MILLINER DS, et al. Combined liver-kidney transplantation for primary hyperoxaluria type 2: a case report[J]. Am J Transplant, 2018, 18(1): 253-257. DOI: 10.1111/ajt.14418. [32] DEL BELLO A, COINTAULT O, DELAS A, et al. Recurrence of oxalate nephropathy after isolated kidney transplantation for primary hyperoxaluria type 2[J]. Am J Transplant, 2018, 18(2): 525-526. DOI: 10.1111/ajt.14550. [33] DEL BELLO A, COINTAULT O, DELAS A, et al. Primary hyperoxaluria type 2 successfully treated with combined liver-kidney transplantation after failure of isolated kidney transplantation[J]. Am J Transplant, 2020, 20(6): 1752-1753. DOI: 10.1111/ajt.15829. [34] JIA Z, ZHONG Q, LIN T, et al. Subsequent liver transplantation did not reverse recurrence of oxalate nephropathy after isolated kidney transplantation for primary type 2 hyperoxaluria[J]. Asian J Surg, 2022, 45(1): 483-485. DOI: 10.1016/j.asjsur.2021.08.066. [35] GENENA KM, SAS DJ, MILLINER DS, et al. Successful treatment of primary hyperoxaluria type 2 with a combined liver and kidney transplant[J]. Kidney Int Rep, 2023, 8(7): 1469-1472. DOI: 10.1016/j.ekir.2023.03.013. [36] YAU AA, HINDI J, URIBARRI J. Recurrent nephrolithiasis causing kidney failure[J]. Am J Kidney Dis, 2021, 77(4): A18-A21. DOI: 10.1053/j.ajkd.2020.04.020. [37] MONICO CG, MILLINER DS. Combined liver-kidney and kidney-alone transplantation in primary hyperoxaluria[J]. Liver Transpl, 2001, 7(11): 954-963. DOI: 10.1053/jlts.2001.28741. [38] SHASHA-LAVSKY H, AVNI A, PAZ Z, et al. Long-term outcomes after pre-emptive liver transplantation in primary hyperoxaluria type 1[J]. Pediatr Nephrol, 2023, 38(6): 1811-1820. DOI: 10.1007/s00467-022-05803-y. -





 下载:
下载: