Comparison of clinical efficacy between tauroursodeoxycholic acid and ursodesoxycholic acid on liver function recovery after liver transplantation
-
摘要:
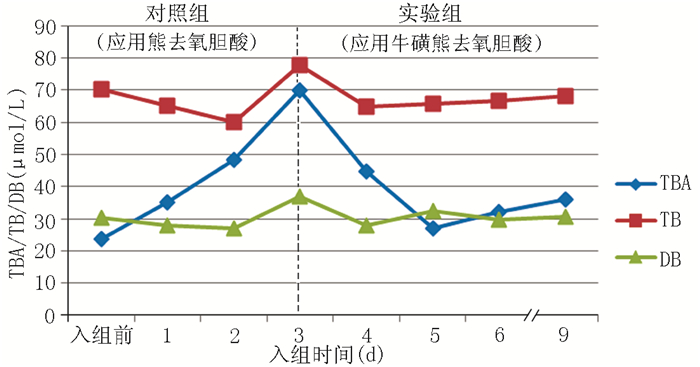
目的 比较牛磺熊去氧胆酸与熊去氧胆酸用于改善肝移植术后肝功能的临床效果。 方法 选择2006年至2012年在首都医科大学附属北京友谊医院接受原位肝移植手术的受者28例,术后即开始口服熊去氧胆酸,治疗3个月转换为口服牛磺熊去氧胆酸6个月。比较入组前,入组后1、2、3、4、5、6、9个月的总胆汁酸(TBA)、总胆红素(TB)、直接胆红素(DB)、丙氨酸转氨酶(ALT)、天冬氨酸转氨酶(AST)、碱性磷酸酶(ALP)、γ-谷氨酰转肽酶(GGT)的变化情况。其中5例分别于入组3个月和9个月行胆汁酸成分测定,比较疏水性胆汁酸与亲水性胆汁酸的变化情况。 结果 应用熊去氧胆酸后,肝功能各项指标在入组3个月内均有所上升。应用牛磺熊去氧胆酸后,与入组3个月比较,TBA在入组5、9个月明显降低;ALT在入组5、6个月时下降;AST在入组4、5个月下降;ALP在入组9个月明显下降;GGT在入组6、9个月下降(均为P < 0.05)。应用牛磺熊去氧胆酸后,患者胆汁酸中亲水性胆汁酸富集,以牛磺熊去氧胆酸为主。 结论 肝移植术后应用牛磺熊去氧胆酸的利胆及保护肝功能作用比熊去氧胆酸更强。 Abstract:Objective To compare the clinical efficacy between tauroursodeoxycholic acid and ursodesoxycholic acid on liver function recovery following liver transplantation. Methods Twenty eight recipients undergoing orthotopic liver transplantation in Beijing Friendship Hospital Affiliated to Capital Medical University from 2006 to 2012 were recruited in this investigation. All patients were orally administered with ursodesoxycholic acid for 3 months and subsequently received oral administration of tauroursodeoxycholic acid for 6 months. The changes in the levels of total bile acid (TBA), total bilirubin (TB), direct bilirubin (DB), alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), γ-glutamyl transpeptidase (GGT) were statistically compared before and 1, 2, 3, 4, 5, 6 and 9 months after enrollment. At 3 and 9 months following enrollment, the components of bile acid were determined in 5 cases to compare the changes between the hydrophobic and hydrophilic bile acid. Results Within 3 months after oral administration of ursodesoxycholic acid, all parameters related to liver function were elevated. Compared with the level at 3 months after enrollment, the level of TBA was significantly decreased at 5 and 9 months after enrollment. The level of ALT declined at 5 and 6 months. The concentration of AST was decreased at 4 and 5 months. The largest decrease in the level of ALP was noted at 9 months. The content of GGT was found to decline at 6 and 9 months (all P < 0.05). After oral administration of tauroursodeoxycholic acid, a higher level of hydrophilic bile acid was detected in the patients' bile acid, dominated by tauroursodeoxycholic acid. Conclusions Tauroursodeoxycholic acid exerts higher clinical efficacy on promoting the secretion of bile and protecting liver function compared with ursodesoxycholic acid after liver transplantation. -
Key words:
- Liver transplantation /
- Cholestasis /
- Tauroursodeoxycholic acid /
- Ursodesoxycholic acid
-
表 1 胆汁淤积患者胆汁酸成分比较(μmol/ml,x±s)
Table 1. Comparison of bile acid composition of patients with cholestasis
胆汁酸成分 n 对照组 实验组 P值 胆酸 5 0.25±0.04 0.53±0.11 0.25 鹅去氧胆酸 5 - - - 去氧胆酸 5 0.28±0.17 0.48±0.40 0.26 甘氨胆酸 5 865±163 1 257±348 0.07 甘氨鹅去氧胆酸 5 584±163 809±315 0.11 甘氨去氧胆酸 5 - - - 甘氨熊去氧胆酸 5 750±468 14±8 0.02 石胆酸 5 0.16±0.03 0.25±0.14 0.42 牛磺胆酸 5 749±462 775±510 0.76 牛磺鹅去氧胆酸 5 364±218 402±108 0.73 牛磺去氧胆酸 5 - - - 牛磺石胆酸 5 0.43±0.31 0.79±0.43 0.15 牛磺熊去氧胆酸 5 197±130 1 811±1 059 0.03 熊去氧胆酸 5 0.37±0.14 - - 注:-为未检出 -
[1] 周尊强, 张正筠, 王书云, 等.肝移植术后远期胆道并发症的诊断与治疗[J].器官移植, 2013, 4(6):347-349. http://www.organtranspl.com/CN/article/downloadArticleFile.do?attachType=PDF&id=8676Zhou ZQ, Zhang ZY, Wang SY, et al. Diagnosis and treatment for long-term biliary complications after liver transplantation[J].Organ Transplant, 2013, 4(6):347-349. http://www.organtranspl.com/CN/article/downloadArticleFile.do?attachType=PDF&id=8676 [2] Palanisamy AP, Taber DJ, Sutter AG, et al. Clinical outcomes and costs associated with in-hospital biliary complications after liver transplantation: a cross-sectional analysis[J]. J Gastrointest Surg, 2015, 19(2):282-289. doi: 10.1007/s11605-014-2675-1 [3] Drzymała-Czyz. S, Jończyk-Potoczna K, Lisowska A, et al. Supplementation of ursodeoxycholic acid improves fat digestion and absorption in cystic fibrosis patients with mild liver involvement[J]. Eur J Gastroenterol Hepatol, 2016, 28(6):645-649. doi: 10.1097/MEG.0000000000000593 [4] 王书云, 唐美华, 陈国庆, 等.肝移植后熊去氧胆酸对肝生物化学指标及胆管并发症影响的临床随机对照研究[J].中华肝脏病杂志, 2014, 22(7):529-535. http://cpfd.cnki.com.cn/Article/CPFDTOTAL-ZHYX201210002106.htmWang SY, Tang MH, Chen GQ, et al. Effect of post-liver transplantation administration of ursodeoxychofic acid on serum liver tests and biliary complications:a randomized clinical trial[J]. Chin J Hepatol, 2014, 22(7):529-535. http://cpfd.cnki.com.cn/Article/CPFDTOTAL-ZHYX201210002106.htm [5] Iijima T, Hoshino J, Suwabe T, et al. Ursodeoxycholic acid for treatment of enlarged polycystic liver[J]. Ther Apher Dial, 2016, 20(1):73-78. doi: 10.1111/tap.2016.20.issue-1 [6] 李伟, 王枫, 吕宗舜, 等.熊去氧胆酸治疗非酒精性脂肪性肝病的系统评价[J].世界华人消化杂志, 2013, 21(23):2335-2343. doi: 10.11569/wcjd.v21.i23.2335Wei L, Feng W, Lyu ZS, et al. Efficacy of ursodesoxycholic acid in treatment of nonalcoholic fatty liver disease: a Meta-analysis. [J]. World Chin J Digestol, 2013, 21(23):2335-2343. doi: 10.11569/wcjd.v21.i23.2335 [7] Cheung AC, Lapointe-Shaw L, Kowgier M, et al. Combined ursodeoxycholic acid (UDCA) and fenofibrate in primary biliary cholangitis patients with incomplete UDCA response may improve outcomes[J]. Aliment Pharmacol Ther, 2016, 43(2):283-293. doi: 10.1111/apt.13465 [8] 陈建飞, 赵期康, 李晋忠, 等.牛磺熊去氧胆酸与熊去氧胆酸对预防保胆术后结石复发的临床研究[J].中国微创外科杂志, 2014, 14(4):311-313. http://www.cnki.com.cn/Article/CJFDTOTAL-ZWWK201404010.htmChen JF, Zhao QK, Li JZ, et al. A comparative clinical study for the relapse of cholelithiasis after gallbladder-preserving lithotomy between tauroursodeoxycholic acid and ursodeoxycholic acid[J]. Chin J Minim Invas Surg, 2014, 14(4):311-313. http://www.cnki.com.cn/Article/CJFDTOTAL-ZWWK201404010.htm [9] Vang S, Longley K, Steer CJ, et al. The unexpected uses of urso-and tauroursodeoxycholic acid in the treatment of non-liver diseases[J]. Glob Adv Health Med, 2014, 3(3):58-69. doi: 10.7453/gahmj.2014.017 [10] Kohli R, Setchell KD, Kirby M, et al. A surgical model in male obese rats uncovers protective effects of bile acids post-bariatric surgery[J]. Endocrinology, 2013, 154(7):2341-2351. doi: 10.1210/en.2012-2069 [11] 杨晓冬, 李晖, 李晓林, 等.牛磺酸熊去氧胆酸治疗慢性乙型肝炎重叠戊型肝炎感染疗效观察[J].中国基层医药, 2014, 21(15):2375-2376. http://d.wanfangdata.com.cn/Periodical/zgjcyy201415067Yang XD, Li H, Li XL, et al. Observation on curative effect of tauroursodeoxycholic acid in the treatment of chronic hepatitis B infection superinfected with hepatitis E infection[J]. Chin J Prim Med Pharm, 2014, 21(15):2375-2376. http://d.wanfangdata.com.cn/Periodical/zgjcyy201415067 [12] 周健, 刘黎, 黄丽雯, 等.牛磺熊去氧胆酸治疗非酒精性脂肪肝疗效观察[J].实用肝脏病杂志, 2014, 17(1):80-81. http://www.cnki.com.cn/Article/CJFDTOTAL-GBSY201401025.htmZhou J, Liu L, Huang LW, et al. Clinical observation of tauroursodeoxycholic acid in treatment of patients with non-alcohol fatty liver[J]. J Clin Hepatol, 2014, 17(1):80-81. http://www.cnki.com.cn/Article/CJFDTOTAL-GBSY201401025.htm [13] Pan XL, Zhao L, Li L, et al. Efficacy and safety of tauroursodeoxycholic acid in the treatment of liver cirrhosis: a double-blind randomized controlled trial[J]. J Huazhong Univ Sci Technolog Med Sci, 2013, 33(2):189-194. doi: 10.1007/s11596-013-1095-x [14] 王文涛, 杨俭, 严律南, 等.熊去氧胆酸对肝移植术后受肝者肝功能异常的治疗作用[J].中华肝脏病杂志, 2012, 20(2):144-145. http://med.wanfangdata.com.cn/Paper/Detail?id=PeriodicalPaper_zhgzbzz201202017Wang WT, Yang J, Yan LN, et al. Ursodeoxycholic acid treatment to resolve abnormal function in liver transplant recipients[J]. Chin J Hepatol, 2012, 20(2):144-145. http://med.wanfangdata.com.cn/Paper/Detail?id=PeriodicalPaper_zhgzbzz201202017 [15] Gohlke H, Schmitz B, Sommerfeld A, et al. α5 β1-integrins are sensors for tauroursodeoxycholic acid in hepatocytes[J]. Hepatology, 2013, 57(3):1117-1129. doi: 10.1002/hep.25992 [16] 曹荣, 胡旭东, 柏涛, 等.熊去氧胆酸与牛磺熊去氧胆酸联合多烯磷脂酰胆碱治疗非酒精性脂肪肝的疗效比较[J].中国药房, 2013, 24(4):365-367. http://www.cnki.com.cn/Article/CJFDTOTAL-ZGYA201304031.htmCao R, Hu XD, Bai T, et al. Comparison of therapeutic efficacy of ursodesoxycholic acid or tauro-ursodesoxycholic acid combined with polyene phosphatidylcholine for non-alcohol fatty liver disease[J]. Chin Pharm, 2013, 24(4):365-367. http://www.cnki.com.cn/Article/CJFDTOTAL-ZGYA201304031.htm [17] Lu H, Lu L, Xu ZC, et al. Tauroursodeoxycholic acid and 4-phenyl butyric acid alleviate endoplasmic reticulum stress and improve prognosis of donation after cardiac death liver transplantation in rats[J]. Hepatobiliary Pancreat Dis Int, 2014, 13(6):586-593. doi: 10.1016/S1499-3872(14)60269-1 [18] 李俊, 陈虹, 范铁艳, 等.肝移植后肝功能的异常[J].中国组织工程研究, 2013, 17(31): 5686-5692. http://www.cnki.com.cn/Article/CJFDTOTAL-XDKF201331021.htmLi J, Chen H, Fan TY, et al. Abnormal liver function after liver transplantation[J]. Clin J Tissue Eng Res, 2013, 17(31): 5686-5692. http://www.cnki.com.cn/Article/CJFDTOTAL-XDKF201331021.htm [19] Tang C, Koulajian K, Schuiki I, et al. Glucose-induced beta cell dysfunction in vivo in rats: link between oxidative stress and endoplasmic reticulum stress[J]. Diabetologia, 2012, 55(5):1366-1379. doi: 10.1007/s00125-012-2474-8 -





 下载:
下载: