-
摘要: 肝移植是目前公认的治疗终末期肝病的最有效措施,但肝供体短缺成为全球移植界面临的难题。如何解决这一问题成为各国科学家研究的重点。本文从人造肝脏的培育历史出发,总结了近年来人造肝脏的研究进展,以期为人造肝脏的研究提供参考。
-
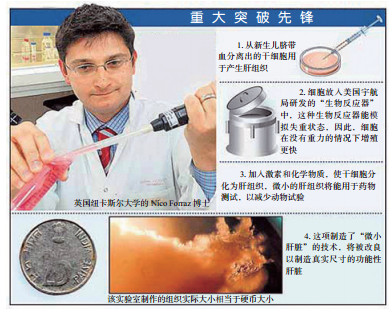
图 1 世界上首个人造肝脏及其发明者Forraz博士[7]
Figure 1. World's first artificial liver and it's creator Dr Forraz
图 2 3D打印的碳水化合物玻璃晶格[10]
Figure 2. 3D printed carbohydrate glass lattice
图 3 2011年Bhatia教授团队构建的人造肝脏示意图[12]
Figure 3. Schematic diagram of artificial liver created by Professor Bhatia teams in 2011
图 4 Bhatia团队构建的人造肝脏“种子”流程图[16]
Figure 4. Flow chart of construction of artificial liver seed grafs created by Bhatia teams
-
[1] Starzl TE, Koep LJ, Halgrimson CG, et al. Fifteen years of clinical liver transplantation[J]. Gastroenterology, 1979, 77(2): 375-388. [2] 中国肝移植年度科学报告[EB/OL]. [2017-07-08]. http://www.cltr.org/pages/index.jsp. [3] 陈规划.中国大陆肝移植:过去、现在和将来[J].器官移植, 2010, 1(1): 5-6. DOI: 10.3969/j.issn.1674-7445.2010.01.001.Chen GH. The past, present and future of liver transplantation in mainland China[J]. Organ Transplant, 2010, 1(1): 5-6. DOI: 10.3969/j.issn.1674-7445.2010.01.001. [4] 中华医学会器官移植学分会, 中国医师协会器官移植医师分会.中国儿童肝移植临床诊疗指南(2015版)[J].临床肝胆病杂志, 2016, 32(7): 1235-1244. DOI: 10.3969/j.issn.1001-5256.2016.07.001.Branch of Organ Transplantation of Chinese Medical Association, Branch of Organ Transplant Physician of Chinese Medical Doctor Association. Clinical guidelines for pediatric liver transplantation in China (2015)[J]. J Clin Hepatol, 2016, 32(7): 1235-1244. DOI: 10.3969/j.issn.1001-5256.2016.07.001. [5] 周霞, 韩英. 干细胞在肝脏疾病治疗中的临床应用及分子机制[J/CD]. 中华细胞与干细胞杂志(电子版), 2015, 5(2): 58-65. DOI: 10.3877/cma.j.issn.2095-1221.2015.02.012.Zhou X, Han Y. Clinical application and molecular mechanisms of stem cell therapy for liver disease[J/CD]. Chin J Cell Stem Cell(Electr Edit), 2015, 5(2): 58-65. DOI: 10.3877/cma.j.issn.2095-1221.2015.02.012. [6] Christensen B. World's first artificial human liver grown in lab[EB/OL]. (2006-10-31)[2017-07-08]. https://www.livescience.com/4276-world-artificial-human-liver-grown-lab.html. [7] British scientists grow human liver in a laboratory[EB/OL]. [2017-07-08]. https://lifeboat.com/ex/bios.nico.forraz. [8] Huang H, Oizumi S, Kojima N, et al. Avidin-biotin binding-based cell seeding and perfusion culture of liver-derived cells in a porous scaffold with a three-dimensional interconnected flow-channel network[J]. Biomaterials, 2007, 28(26): 3815-3823. DOI: 10.1016/j.biomaterials.2007.05.004. [9] Huang Y, He K, Wang X. Rapid prototyping of a hybrid hierarchical polyurethane-cell/hydrogel construct for regenerative medicine[J]. Mater Sci Eng C Mater Biol Appl, 2013, 33(6): 3220-3229. DOI: 10.1016/j.msec.2013.03.048. [10] Miller JS, Stevens KR, Yang MT, et al. Rapid casting of patterned vascular networks for perfusable engineered three-dimensional tissues[J]. Nat Mater, 2012, 11(9): 768-774. DOI: 10.1038/nmat3357. [11] Kizawa H, Nagao E, Shimamura M, et al. Scaffold-free 3D bio-printed human liver tissue stably maintains metabolic functions useful for drug discovery[J]. Biochem Biophys Rep, 2017(10): 186-191. http://www.sciencedirect.com/science/article/pii/S2405580817300596 [12] Chen AA, Thomas DK, Ong LL, et al. Humanized mice with ectopic artificial liver tissues[J]. Proc Natl Acad Sci U S A, 2011, 108(29): 11842-11847. DOI: 10.1073/pnas.1101791108. [13] Trafton A. Engineered liver tissue expands after transplant tiny implantable " seeds" of tissue produce fully functional livers.[EB/OL]. [2017-07-08]. http://news.mit.edu/2017/engineered-liver-tissue-expands-after-transplant-0719. [14] Greene AK, Wiener S, Puder M, et al. Endothelial-directed hepatic regeneration after partial hepatectomy[J]. Ann Surg, 2003, 237(4): 530-535. DOI: 10.1097/01.SLA.0000059986.96051.EA. [15] Baranski JD, Chaturvedi RR, Stevens KR, et al. Geometric control of vascular networks to enhance engineered tissue integration and function[J]. Proc Natl Acad Sci U S A, 2013, 110(19): 7586-7591. DOI: 10.1073/pnas.1217796110. [16] Stevens KR, Ungrin MD, Schwartz RE, et al. InVERT molding for scalable control of tissue microarchitecture[J]. Nat Commun, 2013, 4:1847. DOI: 10.1038/ncomms2853. [17] de Jong YP, Dorner M, Mommersteeg MC, et al. Broadly neutralizing antibodies abrogate established hepatitis C virus infection[J]. Sci Transl Med, 2014, 6(254): 254ra129. DOI: 10.1126/scitranslmed.3009512. [18] Stevens KR, Scull MA, Ramanan V, et al. In situ expansion of engineered human liver tissue in a mouse model of chronic liver disease[J]. Sci Transl Med, 2017, 9(399). DOI: 10.1126/scitranslmed.aah5505. -





 下载:
下载: