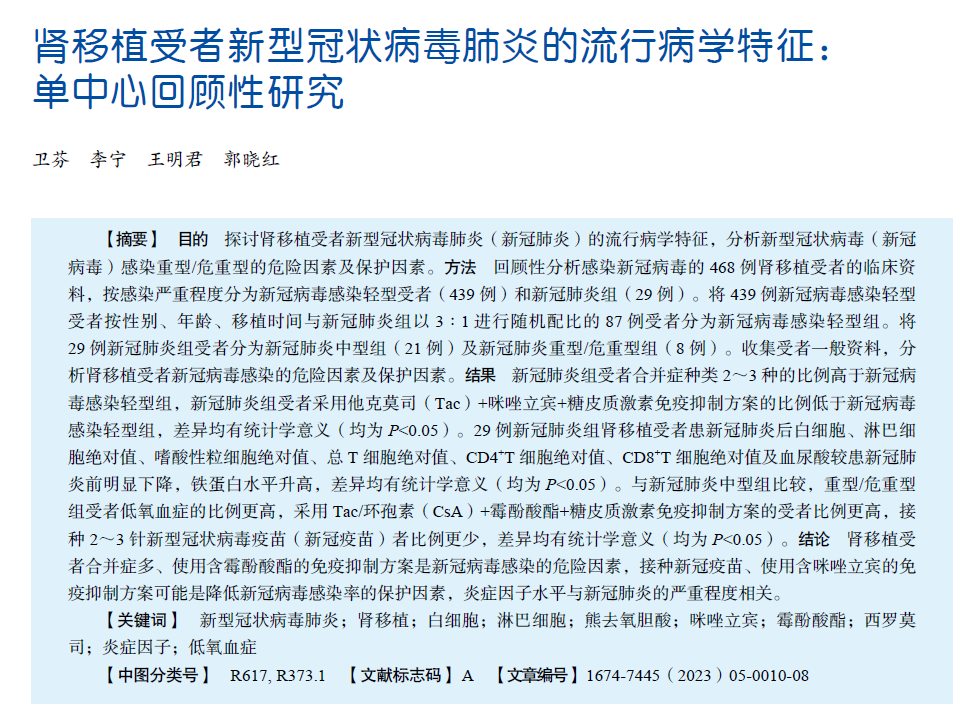
Epidemiological characteristics of SARS-CoV-2 pneumonia in kidney transplant recipients : a single-center retrospective study
-
摘要:
目的 探讨肾移植受者新型冠状病毒肺炎(新冠肺炎)的流行病学特征,分析新型冠状病毒(新冠病毒)感染重型/危重型的危险因素及保护因素。 方法 回顾性分析感染新冠病毒的468例肾移植受者的临床资料,按感染严重程度分为新冠病毒感染轻型受者(439例)和新冠肺炎组(29例)。将439例新冠病毒感染轻型受者按性别、年龄、移植时间与新冠肺炎组以3∶1进行随机配比的87例受者分为新冠病毒感染轻型组。将29例新冠肺炎组受者分为新冠肺炎中型组(21例)及新冠肺炎重型/危重型组(8例)。收集受者一般资料,分析肾移植受者新冠病毒感染的危险因素及保护因素。 结果 新冠肺炎组受者合并症种类2~3种的比例高于新冠病毒感染轻型组,新冠肺炎组受者采用他克莫司(Tac)+咪唑立宾+糖皮质激素免疫抑制方案的比例低于新冠病毒感染轻型组,差异均有统计学意义(均为P<0.05)。29例新冠肺炎组肾移植受者患新冠肺炎后白细胞、淋巴细胞绝对值、嗜酸性粒细胞绝对值、总T细胞绝对值、CD4+T细胞绝对值、CD8+T细胞绝对值及血尿酸较患新冠肺炎前明显下降,铁蛋白水平升高,差异均有统计学意义(均为P<0.05)。与新冠肺炎中型组比较,重型/危重型组受者低氧血症的比例更高,采用Tac/环孢素(CsA)+霉酚酸酯+糖皮质激素免疫抑制方案的受者比例更高,接种2~3针新型冠状病毒疫苗(新冠疫苗)者比例更少,差异均有统计学意义(均为P<0.05)。 结论 肾移植受者合并症多、使用含霉酚酸酯的免疫抑制方案是新冠病毒感染的危险因素,接种新冠疫苗、使用含咪唑立宾的免疫抑制方案可能是降低新冠病毒感染率的保护因素,炎症因子水平与新冠肺炎的严重程度相关。 Abstract:Objective To investigate the epidemiological characteristics of SARS-CoV-2 pneumonia in kidney transplant recipients and analyze the risk and protective factors of severe/critical infection with SARS-CoV-2. Methods Clinical data of 468 kidney transplant recipients infected with SARS-CoV-2 were retrospectively analyzed. According to the severity of infection, they were divided into mild SARS-CoV-2 infection recipients (n=439) and SARS-CoV-2 pneumonia group (n=29). Among the 439 mild SARS-CoV-2 infection recipients, 87 recipients who were randomly matched with their counterparts in the SARS-CoV-2 pneumonia group according to sex, age and transplantation time at a ratio of 3∶1 were allocated into the mild SARS-CoV-2 infection group. Twenty-nine recipients in the SARS-CoV-2 pneumonia group were divided into the moderate SARS-CoV-2 pneumonia group (n=21) and severe/critical SARS-CoV-2 pneumonia group (n=8). Baseline data of all recipients were collected. The risk and protective factors of SARS-CoV-2 infection in kidney transplant recipients were identified. Results The proportion of recipients complicated with 2-3 types of complications in the SARS-CoV-2 pneumonia group was higher than that in the mild SARS-CoV-2 infection group, and the proportion of recipients treated with tacrolimus(Tac)+mizoribine+glucocorticoid immunosuppression regimen in the SARS-CoV-2 pneumonia group was lower than that in the mild SARS-CoV-2 infection group, and significant differences were observed (both P<0.05). In 29 kidney transplant recipients with SARS-CoV-2 pneumonia in the SARS-CoV-2 pneumonia group, white blood cells, the absolute values of lymphocytes, eosinophils, total T cells, CD4+T cells and CD8+T cells, and serum uric acid levels were significantly lower, whereas ferritin levels were significantly higher than the values prior to SARS-CoV-2 pneumonia, and significant differences were observed (all P<0.05). Compared with the moderate SARS-CoV-2 pneumonia group, the proportion of recipients with hypoxemia was higher, the proportion of recipients treated with Tac/ciclosporin (CsA)+mycophenolate mofetil+glucocorticoid immunosuppression regimen was higher, and the proportion of recipients administered with 2-3 doses of SARS-CoV-2 vaccine was lower in the severe/critical SARS-CoV-2 pneumonia group, and significant differences were observed (all P<0.05). Conclusions More complications and immunosuppression regimen containing mycophenolate mofetil are the risk factor for SARS-CoV-2 infection in kidney transplant recipients. Vaccination with SARS-CoV-2 vaccine and immunosuppression regimen containing mizoribine are probably the protective factors for lowering the risk of SARS-CoV-2 infection. The levels of inflammatory cytokines are associated with the severity of SARS-CoV-2 pneumonia. -
表 1 两组受者一般资料比较
Table 1. Comparison of general data between recipients of two groups
变量 新冠病毒感染轻型组(n=87) 新冠肺炎组
(n=29)χ2/t/Z值 P值 术前吸烟史[n(%)] 0.59 0.440 否 66(76) 24(83) 是 21(24) 5(17) 合并症数量①[n(%)] 8.90 0.030 无 24(28) 5(17) 1种 37(43) 9(31) 2~3种 26(30) 15(52) 免疫抑制方案 [n(%)] Tac+霉酚酸酯+糖皮质激素 35(40) 17(59) 2.97 0.130 Tac+咪唑立宾+糖皮质激素 40(46) 5(17) 7.56 0.008 Tac+霉酚酸酯+西罗莫司 3(3) 2(7) 0.07 0.790 Tac+咪唑立宾+西罗莫司 3(3) 2(7) 0.07 0.790 西罗莫司+咪唑立宾 1(1) 1(3) 0 1.000 环孢素+霉酚酸酯 5(6) 2(7) 0 1.000 感染前服用熊去氧胆酸史[n(%)] 44(51) 12(41) 0.74 0.520 感染时熊去氧胆酸服用时间[M(P25, P75),d] 0(0,6.5) 0(0,12.0) −1.06 0.290 疫苗接种[n(%)] 0~1针 31(36) 13(45) 0.86 0.350 2~3针 56(64) 16(55) 0 1.000 注:①合并症包括糖尿病、高血压、冠状动脉粥样硬化性心脏病、恶性肿瘤史及肺部其他疾病。 表 2 肾移植受者患新冠肺炎前后各指标变化
Table 2. Changes of indicators of kidney transplant recipients before and after SARS-CoV-2 pneumonia
变量 发病前
(n=29)发病后
(n=29)t/Z值 P值 白细胞($\bar {{x}} $±s,×109/L) 7.7±2.3 5.7±2.4 3.236 0.002 淋巴细胞绝对值[M(P25, P75),×109/L] 2.2(1.6,2.9) 0.7(0.4,1.1) −5.669 <0.001 嗜酸性粒细胞绝对值[M(P25, P75),×109/L] 0.05(0.03,0.08) 0(0,0.01) −5.503 <0.001 总T细胞绝对值[M(P25, P75),/μL] 1 406(967,1 934) 391(245,569) −5.858 <0.001 CD4+T细胞绝对值[M(P25, P75),/μL] 737(373,1 063) 160(94,291) −5.651 <0.001 CD8+T细胞绝对值[M(P25, P75),/μL] 577(432,905) 229(160,276) −5.036 <0.001 铁蛋白[M(P25, P75),μg/L ] 208(121,228) 609(474,961) −4.871 <0.001 Scr[M(P25, P75),μmol/L] 109(86,144) 125(92,184) −1.151 0.250 血尿酸($\bar {{x}} $±s,μmol/L) 340±64 291±87 2.432 0.018 eGFR[M(P25, P75),mL/min] 55(38,79) 47(34,79) 0.250 0.460 表 3 新冠肺炎中型组与重型/危重型组受者各指标比较
Table 3. Comparison of indicators of recipients between the moderate and the severe/critical SARS-CoV-2 pneumonia group
变量 中型组(n=21) 重型/危重型组(n=8) χ2/t/Z值 P值 高热[n(%)] 14(67) 8(8/8) 1.93 0.16 呼吸道症状[n(%)] 16(76) 6(3/4) 0 1.00 低氧血症[n(%)] 0 7(7/8) 19.70 <0.01 消化道症状[n(%)] 4(19) 2(1/4) 0 1.00 感染至出现肺炎的时间[M(P25, P75),d] 10(8,13) 10(8,15) −0.47 0.64 服用免疫抑制剂类型[n(%)] Tac/CsA+霉酚酸酯+糖皮质激素 11(52) 8(8/8) 9.19 0.01 Tac+咪唑立宾+糖皮质激素 5(24) 0 0.94 0.33 Tac+霉酚酸酯+西罗莫司 2(10) 0 0.01 0.93 Tac+咪唑立宾+西罗莫司 2(10) 0 0.01 0.93 西罗莫司+咪唑立宾+糖皮质激素 1(5) 0 0 1.00 Tac+西罗莫司+糖皮质激素 0 0 0 1.00 服用熊去氧胆酸[n(%)] 10(48) 2(1/4) 0.47 0.49 疫苗接种[n(%)] 8.51 <0.01 0~1针 7(33) 6(3/4) 2~3针 14(67) 2(1/4) 白细胞[M(P25, P75),×109/L] 8(7,9) 7(5,9) −1.22 0.22 淋巴细胞绝对值[M(P25, P75),×109/L] 2.2(1.7,2.9) 2.1(0.9,3.2) −0.51 0.61 总T细胞绝对值[M(P25, P75),/μL] 1 426(1 093,2 100) 994(620,1 628) −1.46 0.15 CD4+T细胞绝对值[M(P25, P75),/μL] 822(453,1 107) 404(283,857) −1.67 0.09 CD8+T细胞绝对值[M(P25, P75),/μL] 618(467,992) 513(304,567) −1.78 0.07 铁蛋白[M(P25, P75),μg/L] 179(110,240) 220(108,266) −0.27 0.79 C-反应蛋白[ M(P25, P75),mg/L] 18(15,51) 23(8,41) −0.54 0.59 降钙素原[ M(P25, P75),ng/L] 4(4,5) 5(4,11) −0.98 0.33 红细胞沉降率[ M(P25, P75),mm/h] 52(25,63) 58(35,76) −0.88 0.33 IL-6 [ M(P25, P75),ng/L] 3.3(2.3,4.5) 3.8(2.3,6.2) −0.32 0.75 D-二聚体[ M(P25, P75),mg/L] 0.30(0.23,0.54) 0.41(0.27,0.64) −1.12 0.26 -
[1] 国家传染病医学中心, 中华医学会器官移植学分会, 中国康复医学会器官移植康复专业委员会, 等. 实体器官移植受者新型冠状病毒感染诊疗专家共识(2023年版)[J]. 器官移植, 2023, 14(2): 163-182. DOI: 10.3969/j.issn.1674-7445.2023.02.001.National Medical Center for Infectious Diseases, Branch of Organ Transplantation of Chinese Medical Association, Organ Transplant Rehabilitation Committee of China Association Rehabilitation Medicine, et al. Expert consensus on diagnosis and treatment of SARS-CoV-2 infection in solid organ transplant recipients (2023 edition)[J]. Organ Transplant, 2023, 14(2): 163-182. DOI: 10.3969/j.issn.1674-7445.2023.02.001. [2] AKALIN E, AZZI Y, BARTASH R, et al. COVID-19 and kidney transplantation[J]. N Engl J Med, 2020, 382(25): 2475-2477. DOI: 10.1056/NEJMc2011117. [3] MAHALINGASIVAM V, SU G, IWAGAMI M, et al. COVID-19 and kidney disease: insights from epidemiology to inform clinical practice[J]. Nat Rev Nephrol, 2022, 18(8): 485-498. DOI: 10.1038/s41581-022-00570-3. [4] DUARSA GWK, SUGIANTO R, YUSARI IGAAA, et al. Method for determining predictor factor for worse outcomes in kidney transplant recipients infected with coronavirus disease 2019 in a systematic review and meta-analysis research[J]. MethodsX, 2023, 11: 102250. DOI: 10.1016/j.mex.2023.102250. [5] PEREIRA MR, MOHAN S, COHEN DJ, et al. COVID-19 in solid organ transplant recipients: initial report from the US epicenter[J]. Am J Transplant, 2020, 20(7): 1800-1808. DOI: 10.1111/ajt.15941. [6] BOSSINI N, ALBERICI F, DELBARBA E, et al. Kidney transplant patients with SARS-CoV-2 infection: the Brescia Renal COVID task force experience[J]. Am J Transplant, 2020, 20(11): 3019-3029. DOI: 10.1111/ajt.16176. [7] WILLICOMBE M, GLEESON S, CLARKE C, et al. Identification of patient characteristics associated with SARS-CoV-2 infection and outcome in kidney transplant patients using serological screening[J]. Transplantation, 2021, 105(1): 151-157. DOI: 10.1097/TP.0000000000003526. [8] 中华人民共和国国家卫生健康委员会办公厅, 中华人民共和国国家中医药管理局综合司. 新型冠状病毒感染诊疗方案(试行第十版)[J]. 中国医药, 2023, 18(2): 161-166. DOI: 10.3760/j.issn.1673-4777.2023.02.001.General Office of National Health Commission of the People's Republic of China, State Administration of Traditional Chinese Medicine General Department of the People's Republic of China. Diagnosis and treatment plan for COVID-19 (the tenth trial edition) [J]. China Med, 2023, 18(2): 161-166. DOI: 10.3760/j.issn.1673-4777.2023.02.001. [9] HILBRANDS LB, DUIVENVOORDEN R, VART P, et al. COVID-19-related mortality in kidney transplant and dialysis patients: results of the ERACODA collaboration [J]. Nephrol Dial Transplant, 2020, 35(11): 1973-1983. DOI: 10.1093/ndt/gfaa261. [10] VILLANEGO F, MAZUECOS A, PÉREZ-FLORES IM, et al. Predictors of severe COVID-19 in kidney transplant recipients in the different epidemic waves: analysis of the Spanish Registry [J]. Am J Transplant, 2021, 21(7): 2573-2582. DOI: 10.1111/ajt.16579. [11] HELDMAN MR, KATES OS, SAFA K, et al. COVID-19 in hospitalized lung and non-lung solid organ transplant recipients: a comparative analysis from a multicenter study [J]. Am J Transplant, 2021, 21(8): 2774-2784. DOI: 10.1111/ajt.16692. [12] CRISTELLI MP, VIANA LA, DANTAS MTC, et al. The full spectrum of COVID-19 development and recovery among kidney transplant recipients [J]. Transplantation, 2021, 105(7): 1433-1444. DOI: 10.1097/TP.0000000000003751. [13] FISHER AM, SCHLAUCH D, MULLOY M, et al. Outcomes of COVID-19 in hospitalized solid organ transplant recipients compared to a matched cohort of non-transplant patients at a national healthcare system in the United States[J]. Clin Transplant, 2021, 35(4): e14216. DOI: 10.1111/ctr.14216. [14] CAILLARD S, CHAVAROT N, FRANCOIS H, et al. Is COVID-19 infection more severe in kidney transplant recipients? [J]. Am J Transplant, 2021, 21(3): 1295-1303. DOI: 10.1111/ajt.16424. [15] KATES OS, HAYDEL BM, FLORMAN SS, et al. Coronavirus disease 2019 in solid organ transplant: a multicenter cohort study[J]. Clin Infect Dis, 2021, 73(11): e4090-e4099. DOI: 10.1093/cid/ciaa1097. [16] COLMENERO J, RODRÍGUEZ-PERÁLVAREZ M, SALCEDO M, et al. Epidemiological pattern, incidence, and outcomes of COVID-19 in liver transplant patients[J]. J Hepatol, 2021, 74(1): 148-155. DOI: 10.1016/j.jhep.2020.07.040. [17] ANGELICO R, BLASI F, MANZIA TM, et al. The management of immunosuppression in kidney transplant recipients with COVID-19 disease: an update and systematic review of the literature[J]. Medicina (Kaunas), 2021, 57(5): 435. DOI: 10.3390/medicina57050435. [18] RAJA MA, MENDOZA MA, VILLAVICENCIO A, et al. COVID-19 in solid organ transplant recipients: a systematic review and meta-analysis of current literature[J]. Transplant Rev (Orlando), 2021, 35(1): 100588. DOI: 10.1016/j.trre.2020.100588. [19] REQUIÃO-MOURA LR, SANDES-FREITAS TV, VIANA LA, et al. High mortality among kidney transplant recipients diagnosed with coronavirus disease 2019: results from the Brazilian multicenter cohort study[J]. PLoS One, 2021, 16(7): e0254822. DOI: 10.1371/journal.pone.0254822. [20] BELLI LS, FONDEVILA C, CORTESI PA, et al. Protective role of tacrolimus, deleterious role of age and comorbidities in liver transplant recipients with COVID-19: results from the ELITA/ELTR multi-center european study[J]. Gastroenterology, 2021, 160(4): 1151-1163. DOI: 10.1053/j.gastro.2020.11.045. [21] 刘琪星, 李月红. 肾移植受者接种新型冠状病毒疫苗的最新进展[J]. 器官移植, 2023, 14(1): 135-141. DOI: 10.3969/j.issn.1674-7445.2023.01.018.LIU QX, LI YH. The latest progress on novel coronavirus vaccination in kidney transplant recipients[J]. Organ Transplant, 2023, 14(1): 135-141. DOI: 10.3969/j.issn.1674-7445.2023.01.018. [22] MA E, AI J, ZHANG Y, et al. Omicron infections profile and vaccination status among 1881 liver transplant recipients: a multi-centre retrospective cohort[J]. Emerg Microbes Infect, 2022, 11(1): 2636-2644. DOI: 10.1080/22221751.2022.2136535. [23] DEMIR E, DHEIR H, SAFAK S, et al. Differences in clinical outcomes of COVID-19 among vaccinated and unvaccinated kidney transplant recipients[J]. Vaccine, 2022, 40(24): 3313-3319. DOI: 10.1016/j.vaccine.2022.04.066. [24] GAO P, LIU J, LIU M. Effect of COVID-19 vaccines on reducing the risk of long COVID in the real world: a systematic review and meta-analysis[J]. Int J Environ Res Public Health, 2022, 19(19): 12422. DOI: 10.3390/ijerph191912422. [25] BREVINI T, MAES M, WEBB GJ, et al. FXR inhibition may protect from SARS-CoV-2 infection by reducing ACE2[J]. Nature, 2023, 615(7950): 134-142. DOI: 10.1038/s41586-022-05594-0. [26] GONG J, DONG H, XIA QS, et al. Correlation analysis between disease severity and inflammation-related parameters in patients with COVID-19: a retrospective study[J]. BMC Infect Dis, 2020, 20(1): 963. DOI: 10.1186/s12879-020-05681-5. [27] LIU J, LI S, LIU J, et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients[J]. EBioMedicine, 2020, 55: 102763. DOI: 10.1016/j.ebiom.2020.102763. [28] CHEN N, ZHOU M, DONG X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study[J]. Lancet, 2020, 395(10223): 507-513. DOI: 10.1016/S0140-6736(20)30211-7. [29] POSTOVSKAYA A, VUJKOVIC A, DE BLOCK T, et al. Leveraging T-cell receptor - epitope recognition models to disentangle unique and cross-reactive T-cell response to SARS-CoV-2 during COVID-19 progression/resolution[J]. Front Immunol, 2023, 14: 1130876. DOI: 10.3389/fimmu.2023.1130876. [30] MCGONAGLE D, SHARIF K, O'REGAN A, et al. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease[J]. Autoimmun Rev, 2020, 19(6): 102537. DOI: 10.1016/j.autrev.2020.102537. [31] PEI G, ZHANG Z, PENG J, et al. Renal involvement and early prognosis in patients with COVID-19 pneumonia[J]. J Am Soc Nephrol, 2020, 31(6): 1157-1165. DOI: 10.1681/ASN.2020030276. [32] CHENG Y, LUO R, WANG K, et al. Kidney disease is associated with in-hospital death of patients with COVID-19[J]. Kidney Int, 2020, 97(5): 829-838. DOI: 10.1016/j.kint.2020.03.005. [33] BROGAN M, ROSS MJ. COVID-19 and kidney disease[J]. Annu Rev Med, 2023, 74: 1-13. DOI: 10.1146/annurev-med-042420-104753. [34] BITENCOURT L, PEDROSA AL, DE BRITO SBCS, et al. COVID-19 and renal diseases: an update[J]. Curr Drug Targets, 2021, 22(1): 52-67. DOI: 10.2174/1389450121999201013151300. [35] ZHANG J, PANG Q, ZHOU T, et al. Risk factors for acute kidney injury in COVID-19 patients: an updated systematic review and meta-analysis[J]. Ren Fail, 2023, 45(1): 2170809. DOI: 10.1080/0886022X.2023.2170809. -





 下载:
下载: