Expression of BZW2 and IVD in hepatocellular carcinoma tissues and effect on prognosis of liver transplant recipients with hepatocellular carcinoma
-
摘要:
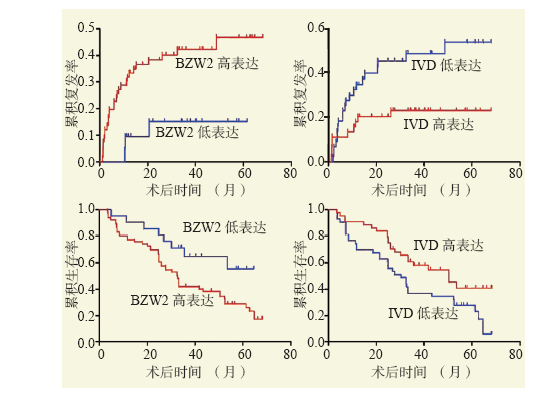
目的 探讨碱性亮氨酸拉链和W2结构域2(BZW2)及异戊酰辅酶A脱氢酶(IVD)在肝细胞癌(肝癌)中的表达及其对肝移植受者预后的影响。 方法 回顾性分析87例肝癌肝移植受者的病理标本及临床资料,分析肝癌肝移植受者术后肿瘤复发转移情况。采用免疫组织化学染色检测BZW2和IVD的表达情况,分析BZW2和IVD与肝癌临床病理参数的关系及其对肝移植术后肿瘤复发和受者预后的影响。 结果 87例受者中,共有31例肿瘤复发,复发率为36%,复发时间为术后2~49个月,复发时间中位数为7个月。免疫组织化学染色结果显示,肝癌组织的BZW2阳性表达率高于正常肝组织(76%比30%),IVD阳性表达率低于正常肝组织(51%比69%),差异均有统计学意义(均为P < 0.01)。BZW2表达与肿瘤直径、有否肿瘤包膜有关(均为P < 0.05),IVD表达与肿瘤直径,甲胎蛋白(AFP)水平,肿瘤、淋巴结、转移(TNM)分期,有否血管侵犯有关(均为P < 0.05)。BZW2高表达组受者肿瘤累积复发率高于BZW2低表达组,累积生存率低于BZW2低表达组;IVD低表达组患者肿瘤累积复发率高于IVD高表达组,累积生存率低于IVD高表达组(均为P < 0.05)。 结论 在肝癌组织中,BZW2蛋白表达水平上调,IVD蛋白表达水平下调。且BZW2高表达和IVD低表达的肝移植受者的累积复发率较高,累积生存率较低。 -
关键词:
- 肝细胞癌 /
- 肝移植 /
- 碱性亮氨酸拉链和W2结构域2(BZW2) /
- 异戊酰辅酶A脱氢酶(IVD) /
- 甲胎蛋白 /
- 血管侵犯 /
- 肿瘤包膜 /
- 肿瘤分期 /
- 肿瘤复发
Abstract:Objective To investigate the expression levels of basic leucine zipper and W2 domain 2 (BZW2) and isovaleryl-CoA dehydrogenase (IVD) in hepatocellular carcinoma (HCC) and evaluate their effect on clinical prognosis of liver transplant recipients with HCC. Methods Pathological specimens and clinical data of 87 liver transplant recipients with HCC were collected and retrospectively analyzed. The recurrence and metastasis of HCC after liver transplantation were assessed. Immunohistochemical staining was used to detect the expression levels of BZW2 and IVD. The relationship between BZW2, IVD and clinicopathological parameters of HCC and their effect on postoperative recurrence and clinical prognosis of the recipients was analyzed. Results Among 87 recipients, 31 cases recurred with a recurrence rate of 36%. HCC recurred at postoperative 2-49 months and the median recurrence time was postoperative 7 months. Immunohistochemical staining demonstrated that the positive expression rate of BZW2 in the HCC tissues was significantly higher than that in normal liver tissues (76% vs. 30%), and the positive expression rate of IVD was significantly lower compared with that in normal liver tissues (51% vs. 69%) (both P < 0.01). BZW2 expression was significantly correlated with tumor diameter and tumor capsule (both P < 0.05), whereas IVD expression was significantly associated with tumor diameter, alpha-fetoprotein (AFP) level, tumor, node and metastasis (TNM) staging and whether vascular invasion was found or not (all P < 0.05). In the high BZW2 expression group, the cumulative recurrence rate of HCC was significantly higher and the cumulative survival rate was significantly lower than those in the low BZW2 expression group. In the low IVD expression group, the cumulative recurrence rate of HCC was significantly higher and the cumulative survival rate was significantly lower compared with those in the high IVD expression group (all P < 0.05). Conclusions The expression level of BZW2 protein is up-regulated, whereas that of IVD protein is down-regulated in the HCC tissues. Moreover, the cumulative recurrence rate of HCC is relatively high and the cumulative survival rate is relatively low in liver transplant recipients with high BZW2 expression and low IVD expression. -
表 1 BZW2和IVD与肝癌肝移植临床病理参数的关系
Table 1. Relationship between BZW2 and IVD and clinicopathological parameters of liver transplantation for hepatocellular carcinoma [n (%)]
项目 n BZW2高表达 P值 IVD高表达 P值 年龄 0.96 0.46 ≤50岁 46 35(76) 25(54) > 50岁 41 31(76) 19(46) 性别 0.07 0.35 男 76 60(79) 40(53) 女 11 6(55) 4(36) 肿瘤直径 0.03 < 0.01 ≤5 cm 53 36(68) 33(62) > 5 cm 34 30(88) 11(32) AFP水平 0.68 < 0.01 ≤400 μg/L 59 44(75) 37(63) > 400 μg/L 28 22(79) 7(25) TNM分期 0.86 < 0.01 Ⅰ~Ⅱ期 65 49(75) 37(57) Ⅲ~Ⅳ期 22 17(77) 7(32) 血管侵犯 0.38 < 0.01 有 21 18(86) 4(19) 无 66 48(73) 40(61) 肿瘤包膜 < 0.01 0.10 有 18 8(44) 6(33) 无 69 58(84) 38(55) 肿瘤数量 0.08 0.19 单发 59 48(81) 27(46) 多发 28 18(64) 17(61) -
[1] ZHENG R, QU C, ZHANG S, et al. Liver cancer incidence and mortality in China: temporal trends and projections to 2030[J]. Chin J Cancer Res, 2018, 30(6)571-579. DOI: 10.21147j.issn.1000-9604.2018.06.01. [2] SIEGEL RL, MILLER KD, JEMAL A. Cancer statistics, 2020[J]. CA Cancer J Clin, 2020, 70(1): 7-30. DOI: 10.3322/caac.21590. [3] FILGUEIRA NA. Hepatocellular carcinoma recurrence after liver transplantation: risk factors, screening and clinical presentation[J]. World J Hepatol, 2019, 11(3): 261-272. DOI: 10.4254/wjh.v11.i3.261. [4] SPOSITO C, CUCCHETTI A, MAZZAFERRO V. Assessing competing risks for death following liver transplantation for hepatocellular carcinoma[J]. Dig Dis Sci, 2019, 64(4): 1001-1007. DOI: 10.1007/s10620-019-05538-1. [5] 王建丰, 曾凯宁, 李海波, 等. 微血管侵犯对肝癌肝移植受者预后影响的临床研究[J]. 器官移植, 2021, 12(3): 309-316. DOI: 10.3969/j.issn.1674-7445.2021.03.009.WANG JF, ZENG KN, LI HB, et al. Clinical study of microvascular invasion on prognosis of recipients after liver transplantation for liver cancer[J]. Organ Transplant, 2021, 12(3): 309-316. DOI: 10.3969/j.issn.1674-7445.2021.03.009. [6] AL-AMERI AAM, WEI X, WEN X, et al. Systematic review: risk prediction models for recurrence of hepatocellular carcinoma after liver transplantation[J]. Transpl Int, 2020, 33(7): 697-712. DOI: 10.1111/tri.13585. [7] WANG F, BRESLIN SJP, QIU W. Novel oncogenes and tumor suppressor genes in hepatocellular carcinoma[J]. Liver Res, 2021, 5(4): 195-203. DOI: 10.1016/j.livres.2021.06.001. [8] NATU A, SINGH A, GUPTA S. Hepatocellular carcinoma: understanding molecular mechanisms for defining potential clinical modalities[J]. World J Hepatol, 2021, 13(11): 1568-1583. DOI: 10.4254/wjh.v13.i11.1568. [9] CHOI W, CZERNIAK B, OCHOA A, et al. Intrinsic basal and luminal subtypes of muscle-invasive bladder cancer[J]. Nat Rev Urol, 2014, 11(7): 400-410. DOI: 10.1038/nrurol.2014.129. [10] SOLOWAY MS. Bladder cancer: lack of progress in bladder cancer--what are the obstacles?[J]. Nat Rev Urol, 2013, 10(1): 5-6. DOI: 10.1038/nrurol.2012.219. [11] GAO H, YU G, ZHANG X, et al. BZW2 gene knockdown induces cell growth inhibition, G1 arrest and apoptosis in muscle-invasive bladder cancers: a microarray pathway analysis[J]. J Cell Mol Med, 2019, 23(6): 3905-3915. DOI: 10.1111/jcmm.14266. [12] CHENG DD, LI SJ, ZHU B, et al. Downregulation of BZW2 inhibits osteosarcoma cell growth by inactivating the Akt/mTOR signaling pathway[J]. Oncol Rep, 2017, 38(4): 2116-2122. DOI: 10.3892/or.2017.5890. [13] HUANG L, CHEN S, FAN H, et al. BZW2 promotes the malignant progression of colorectal cancer via activating the ERK/MAPK pathway[J]. J Cell Physiol, 2020, 235(5): 4834-4842. DOI: 10.1002/jcp.29361. [14] LIU J, YANG T, ZHANG Y, et al. Promotion of BZW2 by LINC00174 through miR-4500 inhibition enhances proliferation and apoptosis evasion in laryngeal papilloma[J]. Cancer Cell Int, 2020, 20: 471. DOI: 10.1186/s12935-020-01559-3. [15] MOHSEN AW, VOCKLEY J. Kinetic and spectral properties of isovaleryl-CoA dehydrogenase and interaction with ligands[J]. Biochimie, 2015, 108: 108-119. DOI: 10.1016/j.biochi.2014.11.007. [16] HYMAN DB, TANAKA K. Isovaleryl-CoA dehydrogenase activity in isovaleric acidemia fibroblasts using an improved tritium release assay[J]. Pediatr Res, 1986, 20(1): 59-61. DOI: 10.1203/00006450-198601000-00017. [17] D'ANNIBALE OM, KOPPES EA, ALODAIB AN, et al. Characterization of variants of uncertain significance in isovaleryl-CoA dehydrogenase identified through newborn screening: an approach for faster analysis[J]. Mol Genet Metab, 2021, 134(1/2): 29-36. DOI: 10.1016/j.ymgme.2021.08.012. [18] LI Y, ZHENG X, ZHU M, et al. MoIVD-mediated leucine catabolism is required for vegetative growth, conidiation and full virulence of the rice blast fungus magnaporthe oryzae[J]. Front Microbiol, 2019, 10: 444. DOI: 10.3389/fmicb.2019.00444. [19] 中华人民共和国国家卫生健康委员会医政医管局. 原发性肝癌诊疗规范(2019年版)[J]. 临床肝胆病杂志, 2020, 36(2): 277-292. DOI: 10.3969/j.issn.1001-5256.2020.02.007.Chinese Journal of Clinical Bureau of Medical Administration, National Health Commission of the People's Republic of China. Guidelines for diagnosis and treatment of primary liver cancer in China (2019 edition)[J]. J Clin Hepatol, 2020, 36(2): 277-292. DOI: 10.3969/j.issn.1001-5256.2020.02.007. [20] 汪国营. 肝癌肝移植相关热点问题探讨[J]. 中山大学学报(医学科学版), 2021, 42(1): 17-23. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSYK202101003.htmWANG GY. Hot issues related to liver transplantation for hepatocellular carcinoma[J]. J Sun Yat-sen Univ (Med Sci), 2021, 42(1): 17-23. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSYK202101003.htm [21] 霍枫, 季茹, 陈建雄. 肝细胞癌肝移植供肝选择策略[J]. 中华消化外科杂志, 2020, 19(2): 135-138. DOI: 10.3760/cma.j.issn.1673-9752.2020.02.005.HUO F, JI R, CHEN JX. Selection of donor liver in liver transplantation for hepatocellular carcinoma[J]. Chin J Dig Surg, 2020, 19(2): 135-138. DOI: 10.3760/cma.j.issn.1673-9752.2020.02.005. [22] VERNA EC, PATEL YA, AGGARWAL A, et al. Liver transplantation for hepatocellular carcinoma: management after the transplant[J]. Am J Transplant. 2020, 20(2): 333-347. DOI: 10.1111/ajt.15697. [23] HOFFMAN D, MEHTA N. Recurrence of hepatocellular carcinoma following liver transplantation[J]. Expert Rev Gastroenterol Hepatol, 2021, 15(1): 91-102. DOI: 10.1080/17474124.2021.1823213. [24] SAMUEL D, COILLY A. Management of patients with liver diseases on the waiting list for transplantation: a major impact to the success of liver transplantation[J]. BMC Med, 2018, 16(1): 113. DOI: 10.1186/s12916-018-1110-y. [25] 刘召波, 栗光明. 肝移植术后肝癌复发防治进展[J]. 临床肝胆病杂志, 2021, 37(2): 267-271. DOI: 10.3969/j.issn.1001-5256.2021.02.006.LIU ZB, LI GM. Advances in the prevention and treatment of hepatocellular carcinoma recurrence after liver transplantation[J]. J Clin Hepatol, 2021, 37(2): 267-271. DOI: 10.3969/j.issn.1001-5256.2021.02.006. [26] SINGH CR, WATANABE R, ZHOU D, et al. Mechanisms of translational regulation by a human eIF5-mimic protein[J]. Nucleic Acids Res, 2011, 39(19): 8314-8328. DOI: 10.1093/nar/gkr339. [27] JIN X, LIAO M, ZHANG L, et al. Role of the novel gene BZW2 in the development of hepatocellular carcinoma[J]. J Cell Physiol, 2019, 234(9): 16592-16600. DOI: 10.1002/jcp.28331. [28] LI G, LU A, CHEN A, et al. BZW2/5MP1 acts as a promising target in hepatocellular carcinoma[J]. J Cancer, 2021, 12(17): 5125-5135. DOI: 10.7150/jca.53282. [29] LIU L, ZHAO J, PENG Y, et al. MiR-let-7a-5p inhibits invasion and migration of hepatoma cells by regulating BZW2 expression[J]. Onco Targets Ther, 2020, 13: 12269-12279. DOI: 10.2147/OTT.S278954. [30] HIROTA T, IZUMI M, WADA S, et al. Vacuolar protein degradation via autophagy provides substrates to amino acid catabolic pathways as an adaptive response to sugar starvation in Arabidopsis thaliana[J]. Plant Cell Physiol, 2018, 59(7): 1363-1376. DOI: 10.1093/pcp/pcy005. [31] SURGER MJ, ANGELOV A, STIER P, et al. Impact of branched-chain amino acid catabolism on fatty acid and alkene biosynthesis in micrococcus luteus[J]. Front Microbiol, 2018, 9: 374. DOI: 10.3389/fmicb.2018.00374. [32] MILLERIOUX Y, MAZET M, BOUYSSOU G, et al. De novo biosynthesis of sterols and fatty acids in the Trypanosoma brucei procyclic form: carbon source preferences and metabolic flux redistributions[J]. PLoS Pathog, 2018, 14(5): e1007116. DOI: 10.1371/journal.ppat.1007116. [33] LEE WC, CHOU HS, WU TJ, et al. Down-regulation of metabolic proteins in hepatocellular carcinoma with portal vein thrombosis[J]. Clin Proteomics, 2017, 14: 29. DOI: 10.1186/s12014-017-9164-y. -





 下载:
下载: