Analysis of risk factors of multidrug-resistant organism infection in lung transplant recipients based on restricted cubic spline model
-
摘要:
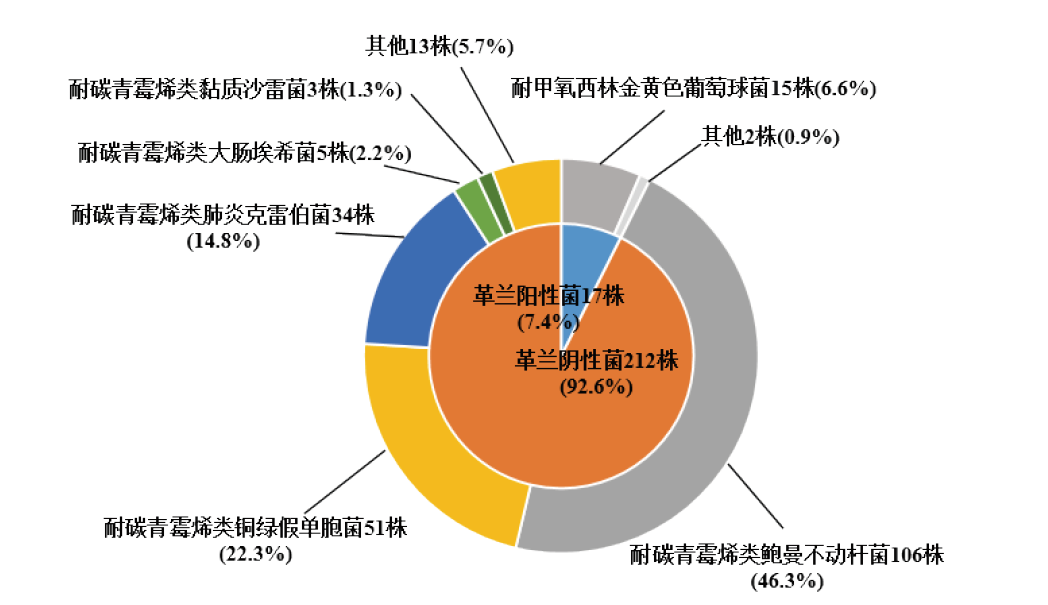
目的 总结肺移植受者术后多重耐药菌(MDRO)的感染现状,分析感染相关危险因素。 方法 回顾性分析321例肺移植受者的临床资料,根据术后是否感染MDRO分为MDRO感染组(122例)和非MDRO感染组(199例)。总结肺移植受者感染MDRO情况,应用logistic回归模型分析肺移植受者感染MDRO的危险因素,结合限制性立方样条模型分析MDRO感染与呼吸机使用时间的剂量-反应关系。 结果 321例肺移植受者中,122例发生MDRO感染,感染率为38.0%。MDRO感染组检出229株病原菌,主要为革兰阴性菌(92.6%),排名前3的分别为耐碳青霉烯类鲍曼不动杆菌(46.3%)、耐碳青霉烯类铜绿假单胞菌(22.3%)和耐碳青霉烯类肺炎克雷伯菌(14.8%)。MDRO感染以下呼吸道感染为主(61.5%),其次为呼吸机相关性肺炎(26.2%)。单因素分析结果显示,采用单肺移植手术方式、术后使用体外膜肺氧合(ECMO)时间长、手术时间长、尿管插管时间长、中心静脉置管时间长、呼吸机使用时间长是肺移植受者MDRO感染的危险因素(均为P < 0.05)。多因素logistic回归分析结果显示,采用单肺移植手术方式、呼吸机使用时间长是肺移植受者MDRO感染的独立危险因素(均为P < 0.05)。限制性立方样条模型分析结果显示,使用呼吸机20 d内,随着呼吸机使用时间的增加,感染风险持续增加;20 d后,延长呼吸机使用时间不增加感染发生的风险,呈现平台效应。 结论 肺移植受者MDRO感染率呈逐年下降趋势,采用单肺移植方式、呼吸机使用时间长是肺移植受者MDRO感染的独立危险因素。 -
关键词:
- 肺移植 /
- 多重耐药菌 /
- 危险因素 /
- 机械通气 /
- 限制性立方样条模型 /
- 耐碳青霉烯类鲍曼不动杆菌 /
- 耐碳青霉烯类铜绿假单胞菌 /
- 耐碳青霉烯类肺炎克雷伯菌
Abstract:Objective To summarize current status of multidrug-resistant organism (MDRO) infection in lung transplant recipients and analyze the risk factors of MDRO infection. Methods Clinical data of 321 lung transplant recipients were retrospectively analyzed. According to the incidence of postoperative MDRO infection, they were divided into the MDRO group (n=122) and non-MDRO infection group (n=199). The incidence of MDRO infection in lung transplant recipients was summarized. The risk factors of MDRO infection in lung transplant recipients were analyzed by logistic regression model. The dose-response relationship between MDRO infection and time of ventilator use was determined by restricted cubic spline model. Results Among 321 lung transplant recipients, 122 cases developed MDRO infection, with an infection rate of 38.0%. Two hundred and twenty-nine strains of pathogenic bacteria were detected in the MDRO infection group, mainly Gram-negative bacteria (92.6%), and the top three strains were carbapenem-resistant acinetobacter baumannii (46.3%), carbapenem-resistant pseudomonas aeruginosa (22.3%) and carbapenem-resistant klebsiella pneumoniae (14.8%), respectively. MDRO infection mainly consisted of lower respiratory tract infection (61.5%), followed by ventilator-associated pneumonia (26.2%). Univariate analysis showed that the risk factors of MDRO infection in lung transplant recipients were single-lung transplantation, long-time postoperative use of extracorporeal membrane oxygenation (ECMO), long operation time, long-time urinary catheterization, long-time central venous catheterization and long-time ventilator use (all P < 0.05). Multivariate logistic regression analysis indicated that single-lung transplantation and long-time ventilator use were the independent risk factors for MDRO infection in lung transplant recipients (both P < 0.05). Results of restricted cubic spline model analysis showed that the risk of infection continued to increase with the prolongation of ventilator use time within 20 d. After 20 d, prolonging the time of ventilator use failed to increase the risk of infection, showing a plateau effect. Conclusions The MDRO infection rate tends to decline in lung transplant recipients year by year. Single-lung transplantation and long-time ventilator use are the independent risk factors for MDRO infection in lung transplant recipients. -
表 1 肺移植受者MDRO感染危险因素的单因素分析
Table 1. Univariate analysis of risk factors for MDRO infection in lung transplant recipients
变量 MDRO感染组
(n=122)非MDRO感染组
(n=199)统计值 P值 年龄(x±s,岁) 54±12 54±14 0.324 0.754 性别[n(%)] 女 34(27.9) 40(20.1) 2.573 0.109 男 88(72.1) 159(79.9) 手术方式[n(%)] 双肺移植 38(31.1) 97(48.7) 9.610 0.002 单肺移植 84(68.9) 102(51.3) 术后应用ECMO时间[M(P25, P75),d] 25(12,34) 19(7,26) 3.396 0.001 手术时间(x±s,h) 6.3±1.6 5.8±1.9 2.663 0.024 术后抗菌药物使用时间[M(P25, P75),d] 11(2,36) 7(2,35) 0.848 0.397 尿管插管时间[M(P25, P75),d] 10(6,22) 5(4,10) 5.591 < 0.001 中心静脉置管时间[M(P25, P75),d] 16(9,33) 11(6,19) 5.756 0.017 呼吸机使用时间[M(P25, P75),d] 7(2,22) 3(1,10) 5.131 < 0.001 表 2 肺移植受者MDRO感染危险因素的多因素logistic分析
Table 2. Multivariate logistic analysis of risk factors for MDRO infection in lung transplant recipients
变量 β值 标准误 Wald χ2值 OR值 95%CI P值 手术方式 0.672 0.307 2.189 1.959 1.078~3.607 0.029 术后应用ECMO时间 0.006 0.003 1.600 1.006 0.999~1.013 0.110 手术时间 -0.011 0.086 -0.134 0.989 0.834~1.168 0.893 尿管插管时间 -0.007 0.008 -0.911 0.993 0.977~1.009 0.362 中心静脉置管时间 0.002 0.005 0.448 1.002 0.993~1.011 0.654 呼吸机使用时间 0.041 0.015 2.660 1.042 1.012~1.074 0.008 -
[1] 王大鹏, 李小杉, 轩晨昊, 等. 肺移植术后机械通气延长的危险因素分析[J]. 器官移植, 2022, 13(6): 797-802. DOI: 10.3969/j.issn.1674-7445.2022.06.016.WANG DP, LI XS, XUAN CH, et al. Analysis of risk factors of prolonged mechanical ventilation after lung transplantation[J]. Organ Transplant, 2022, 13(6): 797-802. DOI: 10.3969/j.issn.1674-7445.2022.06.016. [2] SOLE A. Multiresistant organisms: bacteria and beyond[J]. Curr Opin Organ Transplant, 2022, 27(3): 184-190. DOI: 10.1097/MOT.0000000000000976. [3] MCCORT M, MACKENZIE E, PURSELL K, et al. Bacterial infections in lung transplantation[J]. J Thorac Dis, 2021, 13(11): 6654-6672. DOI: 10.21037/jtd-2021-12. [4] WU B, HUANG M, JIAO G, et al. Lung transplantation during the outbreak of Coronavirus Disease 2019 in China[J]. J Thorac Cardiovasc Surg, 2022, 163(1): 326-335. DOI: 10.1016/j.jtcvs.2020.10.154. [5] 焦国慧, 王梓涛, 陈静瑜. 肺移植全球发展概况与展望[J]. 器官移植, 2022, 13(4): 417-424. DOI: 10.3969/j.issn.1674-7445.2022.04.002.JIAO GH, WANG ZT, CHEN JY, et al. Current status and prospect of global development of lung transplantation[J]. Organ Transplant, 2022, 13(4): 417-424. DOI: 10.3969/j.issn.1674-7445.2022.04.002. [6] 白镓玮, 马承泰, 吴淼, 等. 肺移植术后多重耐药菌感染的防治研究进展[J]. 武汉大学学报(医学版), 2021, 42(4): 551-557. DOI: 10.14188/j.1671-8852.2021.6010.BAI JW, MA CT, WU M, et al. Research progress in the prevention and treatment of multidrug-resistant organisms infection after lung transplantation[J]. Med J Wuhan Univ, 2021, 42(4): 551-557. DOI: 10.14188/j.1671-8852.2021.6010. [7] JIN M, ZENG L, ZHANG W, et al. Clinical features of multidrug-resistant organism infections in early postoperative solid organ transplantation in a single center[J]. Ann Palliat Med, 2021, 10(4): 4555-4562. DOI: 10.21037/apm-21-777. [8] 赵建兰, 许东风, 赵静, 等. 老年肺部感染住院患者多药耐药菌感染影响因素的回顾性调查[J]. 中华医院感染学杂志, 2019, 29(6): 835-838. DOI: 10.11816/cn.ni.2019-180552.ZHAO JL, XU DF, ZHAO J, et al. Retrospective survey of influencing factors for multidrug-resistant organisms infections in elderly hospitalized patients with pulmonary infections[J]. Chin J Nosocomiol, 2019, 29(6): 835-838. DOI: 10.11816/cn.ni.2019-180552. [9] 方翊天, 吴若林, 黄帆, 等. 肝移植术后多重耐药菌感染危险因素的单中心临床研究[J]. 器官移植, 2021, 12(2): 197-202. DOI: 10.3969/j.issn.1674-7445.2021.02.010.FANG YT, WU RL, HUANG F, et al. Risk factors of multi-drug resistant organism infection after liver transplantation: a single-center clinical trial[J]. Organ Transplant, 2021, 12(2): 197-202. DOI: 10.3969/j.issn.1674-7445.2021.02.010. [10] GAGLIOTTI C, MORSILLO F, MORO ML, et al. Infections in liver and lung transplant recipients: a national prospective cohort[J]. Eur J Clin Microbiol Infect Dis, 2018, 37(3): 399-407. DOI: 10.1007/s10096-018-3183-0. [11] VAN DELDEN C, STAMPF S, HIRSCH HH, et al. Burden and timeline of infectious diseases in the first year after solid organ transplantation in the Swiss transplant cohort study[J]. Clin Infect Dis, 2020, 71(7): e159-e169. DOI: 10.1093/cid/ciz1113. [12] SHAH P, NEUJAHR DC. Lung transplantation: candidate selection and timing of transplant[J]. Curr Opin Organ Transplant, 2021, 26(3): 302-308. DOI: 10.1097/MOT.0000000000000879. [13] CHANG SH, CHAN J, PATTERSON GA. History of lung transplantation[J]. Clin Chest Med, 2023, 44(1): 1-13. DOI: 10.1016/j.ccm.2022.11.004. [14] SHERRY NL, GORRIE CL, KWONG JC, et al. Multisite implementation of whole genome sequencing for hospital infection control: a prospective genomic epidemiological analysis[J]. Lancet Reg Health West Pac, 2022, 23: 100446. DOI: 10.1016/j.lanwpc.2022.100446. [15] TEBANO G, GENEVE C, TANAKA S, et al. Epidemiology and risk factors of multidrug-resistant bacteria in respiratory samples after lung transplantation[J]. Transpl Infect Dis, 2016, 18(1): 22-30. DOI: 10.1111/tid.12471. [16] OH DH, KIM YC, KIM EJ, et al. Multidrug-resistant acinetobacter baumannii infection in lung transplant recipients: risk factors and prognosis[J]. Infect Dis (Lond), 2019, 51(7): 493-501. DOI: 10.1080/23744235.2018.1556400. [17] IBRAHIM S, AL-SARYI N, AL-KADMY IMS, et al. Multidrug-resistant acinetobacter baumannii as an emerging concern in hospitals[J]. Mol Biol Rep, 2021, 48(10): 6987-6998. DOI: 10.1007/s11033-021-06690-6. [18] WOJARSKI J, OCHMAN M, MEDRALA W, et al. Bacterial infections during hospital stay and their impact on mortality after lung transplantation: a single-center study[J]. Transplant Proc, 2018, 50(7): 2064-2069. DOI: 10.1016/j.transproceed.2017.11.080. [19] LIU YF, LIU Y, CHEN X, et al. Epidemiology, drug resistance, and risk factors for mortality among hematopoietic stem cell transplantation recipients with hospital-acquired klebsiella pneumoniae infections: a single-center retrospective study from China[J]. Infect Drug Resist, 2022, 15: 5011-5021. DOI: 10.2147/IDR.S376763. [20] MENG D, CHANG R, ZHU R. Analysis of nosocomial infection and risk factors in lung transplant patients: a case-control study[J]. Ann Transl Med, 2022, 10(14): 804. DOI: 10.21037/atm-22-3023. [21] 杨启文, 吴安华, 胡必杰, 等. 临床重要耐药菌感染传播防控策略专家共识[J]. 中国感染控制杂志, 2021, 20(1): 1-14. DOI: 10.12138/j.issn.1671-9638.20218124.YANG QW, WU AH, HU BJ, et al. Expert consensus on strategies for the prevention and control of spread of clinically important antimicrobial-resistant organisms[J]. Chin J Infect Control, 2021, 20(1): 1-14. DOI: 10.12138/j.issn.1671-9638.20218124. [22] DING D, ZHANG R. China's COVID-19 control strategy and its impact on the global pandemic[J]. Front Public Health, 2022, 10: 857003. DOI: 10.3389/fpubh.2022.857003. [23] KING CS, MANNEM H, KUKREJA J, et al. Lung transplantation for patients with COVID-19[J]. Chest, 2022, 161(1): 169-178. DOI: 10.1016/j.chest.2021.08.041. [24] KHUSH KK, POTENA L, CHERIKH WS, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: 37th adult heart transplantation report-2020; focus on deceased donor characteristics[J]. J Heart Lung Transplant, 2020, 39(10): 1003-1015. DOI: 10.1016/j.healun.2020.07.010. [25] VAN DEN HOOGEN MWF, SEGHERS L, MANINTVELD OC, et al. Care for the organ transplant recipient on the intensive care unit[J]. J Crit Care, 2021, 64: 37-44. DOI: 10.1016/j.jcrc.2021.03.003. [26] VALENTINE VG, BONVILLAIN RW, GUPTA MR, et al. Infections in lung allograft recipients: ganciclovir era[J]. J Heart Lung Transplant, 2008, 27(5): 528-535. DOI: 10.1016/j.healun.2007.12.013. [27] WILSON-SMITH AR, KIM YS, EVANS GE, et al. Single versus double lung transplantation for fibrotic disease-systematic review[J]. Ann Cardiothorac Surg, 2020, 9(1): 10-19. DOI: 10.21037/acs.2019.12.04. [28] DE OLIVEIRA NC, OSAKI S, MALONEY J, et al. Lung transplant for interstitial lung disease: outcomes for single versus bilateral lung transplantation[J]. Interact Cardiovasc Thorac Surg, 2012, 14(3): 263-267. DOI: 10.1093/icvts/ivr085. [29] WEI D, GAO F, WU B, et al. Single versus bilateral lung transplantation for idiopathic pulmonary fibrosis[J]. Clin Respir J, 2019, 13(6): 376-383. DOI: 10.1111/crj.13020. [30] DI NARDO M, TIKKANEN J, HUSAIN S, et al. Postoperative management of lung transplant recipients in the intensive care unit[J]. Anesthesiology, 2022, 136(3): 482-499. DOI: 10.1097/ALN.0000000000004054. [31] YANG Y, CHI Y, YUAN S, et al. The relationship between ventilatory ratio (VR) and 28-day hospital mortality by restricted cubic splines (RCS) in 14, 328 mechanically ventilated ICU patients[J]. BMC Pulm Med, 2022, 22(1): 229. DOI: 10.1186/s12890-022-02019-6. [32] BARNES L, REED RM, PAREKH KR, et al. Mechanical ventilation for the lung transplant recipient[J]. Curr Pulmonol Rep, 2015, 4(2): 88-96. DOI: 10.1007/s13665-015-0114-8. [33] 黄海燕, 罗健, 徐玉兰, 等. 渐进式直立活动对ICU呼吸机依赖患者成功撤机的影响[J]. 护理学杂志, 2014, 29(24): 19-21. DOI: 10.3870/hlxzz.2014.24.019.HUANG HY, LUO J, XU YL, et al. Effect of gradual upright activities on weaning of ICU patients depending on ventilators[J]. J Nurs Sci, 2014, 29(24): 19-21. DOI: 10.3870/hlxzz.2014.24.019. [34] LANGER D. Rehabilitation in patients before and after lung transplantation[J]. Respiration, 2015, 89(5): 353-362. DOI: 10.1159/000430451. [35] 钟海莲, 王迎斌. 呼吸力学监测指导COPD患者机械通气的研究进展[J]. 解放军医学杂志, 2022, 47(12): 1262-1267. DOI: 10.11855/j.issn.0577-7402.2022.12.1262.ZHONG HL, WANG YB. Research progress of respiratory mechanics monitoring in guiding mechanical ventilation of patients with COPD[J]. Med J Chin PLA, 2022, 47(12): 1262-1267. DOI: 10.11855/j.issn.0577-7402.2022.12.1262. -





 下载:
下载: