CRRT combined with immunoabsorption and plasma exchange in treatment of AMR complicated with multiple organ failure after renal transplantation
-
摘要:
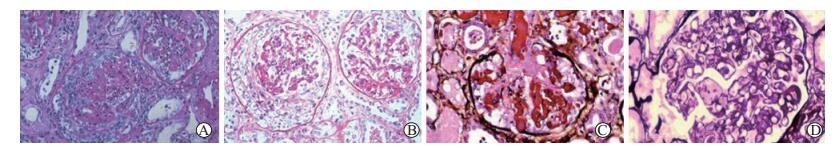
目的 探讨应用连续性肾脏替代治疗(CRRT)联合免疫吸附和血浆置换治疗肾移植术后抗体介导的排斥反应(AMR)合并多器官功能衰竭的效果。 方法 将28例肾移植术后诊断为AMR合并多器官功能衰竭的患者随机分为2组, 对照组(12例)和治疗组(16例)。两组患者均给予甲泼尼龙0.8 g/d冲击治疗5 d, 口服环孢素1.5 mg/(kg·d), CRRT以及强心、利尿等对症治疗; 治疗组在治疗后第7、10日给予免疫吸附和血浆置换治疗。比较两组患者治疗后的总体情况; 比较两组患者治疗前后肾功能[血尿素氮(BUN)、血清肌酐(Scr)]和血电解质的变化; 分析两组患者治疗前后肾组织病理学检查和免疫组织化学(免疫组化)染色结果。 结果 28例患者中, 临床治愈24例, 其中治疗组14例, 对照组10例; 3例恶化, 其中治疗组2例, 对照组1例; 对照组1例死于脑出血。治疗7、12 d后, 治疗组和对照组患者的BUN和Scr水平比较, 差异均有统计学意义(P < 0.05~0.01)。治疗组和对照组的血钠和血钾治疗前后比较, 差异均有统计学意义(P < 0.05~0.01)。肾组织病理学检查显示, 治疗12 d后, 治疗组和对照组患者的移植肾组织浸润的淋巴细胞减少, 血管炎减轻; 与对照组比较, 治疗组的肾小球、小管间质及血管的病理评分均较低, 差异均有统计学意义(均为P < 0.01)。免疫组化染色结果显示, 治疗12 d后, 两组患者的移植肾组织ED1阳性的单核细胞减少, 且治疗组ED1阳性的单核细胞减少更为明显; 治疗12 d后, 治疗组患者肾小管间质的CD4+/CD8+细胞比值比对照组更低, 差异有统计学意义(P < 0.01)。 结论 CRRT联合免疫吸附和血浆置换组合治疗是治疗肾移植术后AMR合并多器官功能衰竭的有效方法。 -
关键词:
- 肾移植 /
- 急性排斥反应 /
- 抗体介导的排斥反应(AMR) /
- 多器官功能衰竭 /
- 连续性肾脏替代治疗(CRRT) /
- 免疫吸附 /
- 血浆置换
Abstract:Objective To investigate the clinical efficacy of continuous renal replacement therapy (CRRT) combined with immunoabsorption and plasma exchange in the treatment of antibody-mediated rejection (AMR) complicated with multiple organ failure after renal transplantation. Methods Twenty-eight patients diagnosed with AMR complicated with multiple organ failure after renal transplantation were randomly divided into the control group (n=12) and treatment group (n=16).All patients were given with methylprednisolone 0.8 g/d shock therapy for 5 d, oral intake of ciclosporin 1.5 mg/(kg·d), CRRT, cardiotonics, diuretics and other symptomatic treatments.In the treatment group, immunoabsorption and plasma exchange were delivered on the 7th and 10th d after treatment.The overall conditions were statistically compared between two groups.The changes of renal function [blood urea nitrogen (BUN), serum creatinine (Scr)] and blood electrolyte before and after treatment were compared between two groups.The results of histopathological examination and immunohistochemical staining of the renal tissues before and after treatment were analyzed in two groups. Results Among 28 patients, 24 cases were clinically cured, including 14 in the treatment group and 10 in the control group.The symptoms of 3 patients were deteriorated, including 2 in the treatment group and 1 in the control group.One patient in the control group died of cerebral hemorrhage.After 7 d and 12 d treatment, the levels of BUN and Scr significantly differed between the treatment group and control group (P < 0.05-0.01).The levels of blood sodium and potassium significantly differed between two groups before and after treatment (P < 0.05-0.01).Pathological examination of renal tissue demonstrated that after 12 d treatment, the number of lymphocytes infiltrated in the transplanted kidney tissues was reduced and the degree of vasculitis was alleviated in two groups.Compared with the control group, the pathological scores of glomerulus, tubulointerstitial and blood vessels were significantly lower in the treatment group (all P < 0.01).Immunohistochemical staining revealed that after 12 d treatment, the number of ED1-positive monocytes in the transplanted kidney tissues was declined in both groups, especially in the treatment group.Following 12 d treatment, the ratio of CD4+/CD8+ cells in renal tubulointerstitial in the treatment group was significantly lower than that in the control group (P < 0.01). Conclusions CRRT combined with immunoabsorption and plasma exchange is an effective method to treat AMR complicated with multiple organ failure following renal transplantation. -
表 1 两组患者治疗前后移植肾组织病理学评分和CD4+/CD8+细胞比值的比较
Table 1. Comparison of histopathological scores and the ratio of CD4+/CD8+ cells of renal allograft of patients between two groups before and after treatment(x±s)
组别 n 病理学评分(分) CD4+/CD8+细胞比值 肾小球 肾小管间质 血管 肾小球 肾小管间质 血管 对照组 治疗前 12 2.8±0.4 2.5±0.7 2.4±0.3 3.1±0.5 5.5±0.4 4.4±0.8 治疗后 11 2.0±0.3a 1.9±0.4a 1.7±0.6a 2.0±0.6a 2.5±0.7a 2.2±0.5a 治疗组 16 治疗前 2.5±0.6 2.4±0.7 2.6±0.3 2.9±0.3 5.8±0.9 4.6±0.5 治疗后 1.3±0.4a, b 1.2±0.3a, b 1.2±0.3a, b 1.7±0.8a 1.9±0.4a, b 1.7±0.5a 与治疗前比较, aP < 0.05;与对照组比较, bP < 0.01 -
[1] LEE JM, LEE SA, CHO HJ, et al.Impact of perioperative renal dysfunction in heart transplantation:combined heart and kidney transplantation could help to reduce postoperative mortality[J].Ann Transplant, 2013, 18:533-549.DOI: 10.12659/AOT.889103. [2] XU C, CARLSSON DO, MIHRANYAN A.Feasibility of using DNA-immobilized nanocellulose-based immunoadsorbent for systemic lupus erythematosus plasmapheresis[J].Colloids Surf B Biointerfaces, 2016, 143:1-6.DOI: 10.1016/j.colsurfb.2016.03.014. [3] HAAS M, LOUPY A, LEFAUCHEUR C, et al.The Banff 2017 Kidney Meeting Report:revised diagnostic criteria for chronic active T cell-mediated rejection, antibody-mediated rejection, and prospects for integrative endpoints for next-generation clinical trials[J].Am J Transplant, 2018, 18(2):293-307.DOI: 10.1111/ajt.14625. [4] AUBERT O, LOUPY A, HIDALGO L, et al.Antibody-mediated rejection due to preexisting versus de novo donor-specific antibodies in kidney allograft recipients[J].J Am Soc Nephrol, 2017, 28(6):1912-1923.DOI: 10.1681/ASN.2016070797. [5] SKRIAPA L, ZISIMOPOULOU P, TRAKAS N, et al.Expression of extracellular domains of muscle specific kinase (MuSK) and use as immunoadsorbents for the development of an antigen-specific therapy[J].J Neuroimmunol, 2014, 276(1/2):150-158.DOI: 10.1016/j.jneuroim.2014.09.013. [6] KIM J, CHOI SE, LIM BJ, et al.Clinical significance of macrophage polarization in antibody-mediated rejection of renal allograft[J].Transplant Proc, 2018, 50(4):1005-1008.DOI: 10.1016/j.transproceed.2018.02.037. [7] EINECKE G, BRÄSEN JH, HANKE N, et al.Fatal pneumococcus sepsis after treatment of late antibody-mediated kidney graft rejection[J].Case Rep Nephrol, 2018:1415450.DOI: 10.1155/2018/1415450. [8] LAN JH, GJERTSON D, ZHENG Y, et al.Clinical utility of complement-dependent C3d assay in kidney recipients presenting with late allograft dysfunction[J].Am J Transplant, 2018, DOI:10.1111/ajt.14871[Epubahead of print]. [9] REDONDO-PACHÓN D, PÉREZ-SÁEZ MJ, MIR M, et al.Impact of persistent and cleared preformed HLA DSA on kidney transplant outcomes[J].Hum Immunol, 2018, 79(6):424-431.DOI: 10.1016/j.humimm.2018.02.014. [10] MONTGOMERY RA, LOUPY A, SEGEV DL.Antibody-mediated rejection:new approaches in prevention and management[J].Am J Transplant, 2018, 18(Suppl 3):3-17.DOI: 10.1111/ajt.14584. [11] 罗子寰, 孙启全.肾移植基础研究2016年盘点[J].器官移植, 2017, 8(1):15-21.DOI:10.3969/j.issn.1674- 7445.2017.01.004.LUO ZH, SUN QQ.Summary of basic study on renal transplantation in 2016[J].Organ Transplant, 2017, 8(1):15-21.DOI: 10.3969/j.issn.1674-7445.2017.01.004. [12] BAILLY E, ANGLICHEAU D, BLANCHO G, et al.Prognostic value of the persistence of C1q-binding anti-HLA antibodies in acute antibody-mediated rejection in kidney transplantation[J].Transplantation, 2018, 102(4):688-698.DOI: 10.1097/TP.0000000000002002. [13] MORESO F, CRESPO M, RUIZ JC, et al.Treatment of chronic antibody mediated rejection with intravenous immunoglobulins and rituximab:a multicenter, prospective, randomized, double-blind clinical trial[J].Am J Transplant, 2018, 18(4):927-935.DOI: 10.1111/ajt.14520. [14] GARG N, SAMANIEGO MD, CLARK D, et al.Defining the phenotype of antibody-mediated rejection in kidney transplantation:advances in diagnosis of antibody injury[J].Transplant Rev (Orlando), 2017, 31(4):257-267.DOI: 10.1016/j.trre.2017.08.005. [15] SOUTH AM, MAESTRETTI L, KAMBHAM N, et al.Persistent C4d and antibody-mediated rejection in pediatric renal transplant patients[J].Pediatr Transplant, 2017, 21(7).DOI: 10.1111/petr.13035. [16] MATIGNON M, PILON C, COMMEREUC M, et al.Intravenous immunoglobulin therapy in kidney transplant recipients with de novo DSA:results of an observational study[J].PLoS One, 2017, 12(6):e0178572.DOI: 10.1371/journal.pone.0178572. [17] PARKES MD, HALLORAN PF, HIDALGO LG.Mechanistic sharing between NK cells in ABMR and effector T cells in TCMR[J].Am J Transplant, 2018, 18(1):63-73.DOI: 10.1111/ajt.14410. [18] LACHMANN N, DUERR M, SCHÖNEMANN C, et al.Treatment of antibody-mediated renal allograft rejection:improving step by step[J].J Immunol Res, 2017:6872046.DOI: 10.1155/2017/6872046. [19] WU GS, CRUZ RJ JR, CAI JC.Acute antibody-mediated rejection after intestinal transplantation[J].World J Transplant, 2016, 6(4):719-728.DOI: 10.5500/wjt.v6.i4.719. [20] HIRANO R, HIRATA N.Immunoadsorption using immusorba TR and PH[J].Transfus Apher Sci, 2017, 56(5):661-665.DOI: 10.1016/j.transci.2017.08.011. -





 下载:
下载: